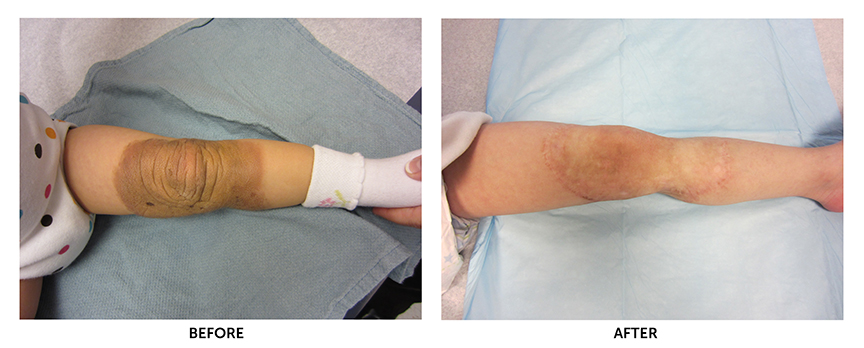
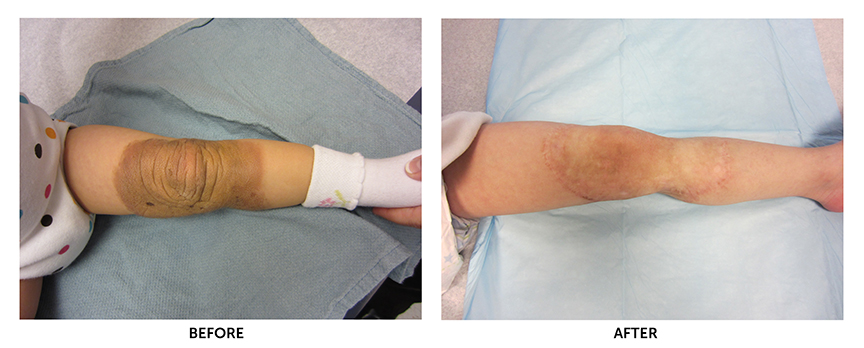
Excision of the nevus in multiple stages, including tissue expansion of the lower abdomen and use of the extra skin for full thickness skin grafting of the nevus defect.
Birthmarks are no longer dismissed as “beauty marks” by laypeople. With skin cancer incidence on the rise (over 74,000 new cases in the United States annually) and the availability of patient education and resources, more pediatricians, patients and families are proactively receiving specialized nevus care than ever before.
There are several types of nevi, defined primarily by color/pigmentation and size. According to nevus.org (an outreach organization dedicated to providing congenital melanocytic nevi education and support), smaller, congenital, pigmented or melanocytic nevi affect one in 50 to 100 people and are typically not problematic.
Large and giant nevi, however, are rare and require a watchful eye. Large nevi appear in around 1 out of every 20,000 births. They typically require more than one surgical excision to remove, and either cover more than 2 percent of the patient’s total body surface area or are larger than the palm of the patient's hand. These lesions also cover a large portion of a major anatomical site, such as the head, legs or arms.
Giant nevi are more rare, appearing in 1 out of every 50,000 births. These nevi cover a very large part of the body and usually involve the torso. Giant nevi are typically accompanied by a number of satellite nevi; together, these features tend to suggest a diagnosis of a large or giant congenital melanocytic nevus.
Community practice vs. hospital for nevus removal
According to Boston Children’s Hospital’s Amir Taghinia, MD, an attending surgeon in the hospital's Department of Plastic and Oral Surgery, certain symptoms—pain, swelling, bleeding or apparent growth of a nevus—call for referral to a specialist for closer examination and possibly a skin biopsy.
Taghinia explains that a nevus that covers a large area—such as an entire forearm, or part of the leg or face—are generally too complex to be addressed in a community practice.
“A pediatric hospital can bring in multiple specialties, such as dermatology and plastic surgery, and provide highly specialized plastic surgical care, such as free tissue transfer and tissue expansion,” he says. “If the lesion is dangerous, if it is precancerous or cancerous, a pediatric hospital has the expertise, knowledge and resources to take the case one step further and provide comprehensive care.”
 Even patients with small nevi requiring simple excisions are best served in a hospital setting with ready access to pediatric anesthesiologists and pain specialists, he says. "A simple excision typically takes about a half hour to 45 minutes. It is difficult to perform on a three-year-old, for example, because it is painful, and the child cannot stay still."
Even patients with small nevi requiring simple excisions are best served in a hospital setting with ready access to pediatric anesthesiologists and pain specialists, he says. "A simple excision typically takes about a half hour to 45 minutes. It is difficult to perform on a three-year-old, for example, because it is painful, and the child cannot stay still."
Equally important as appropriate pain control is appropriate skin closure. Small, large and giant nevus removals all come with a risk of scarring, which can be minimized with the right closure techniques. Because large and giant nevi are so rare, with children, experience removing nevi plays a significant role in scar reduction as well, which also argues for opting for care at a pediatric hospital. “The more procedures you do, the better you are at it,” Taghinia says.
If you have questions about nevus care or wish to refer a patient for evaluation, contact Boston Children’s Department of Plastic and Oral Surgery at 617-355-7252.


 Even patients with small nevi requiring simple excisions are best served in a hospital setting with ready access to pediatric anesthesiologists and pain specialists, he says. "A simple excision typically takes about a half hour to 45 minutes. It is difficult to perform on a three-year-old, for example, because it is painful, and the child cannot stay still."
Even patients with small nevi requiring simple excisions are best served in a hospital setting with ready access to pediatric anesthesiologists and pain specialists, he says. "A simple excision typically takes about a half hour to 45 minutes. It is difficult to perform on a three-year-old, for example, because it is painful, and the child cannot stay still."