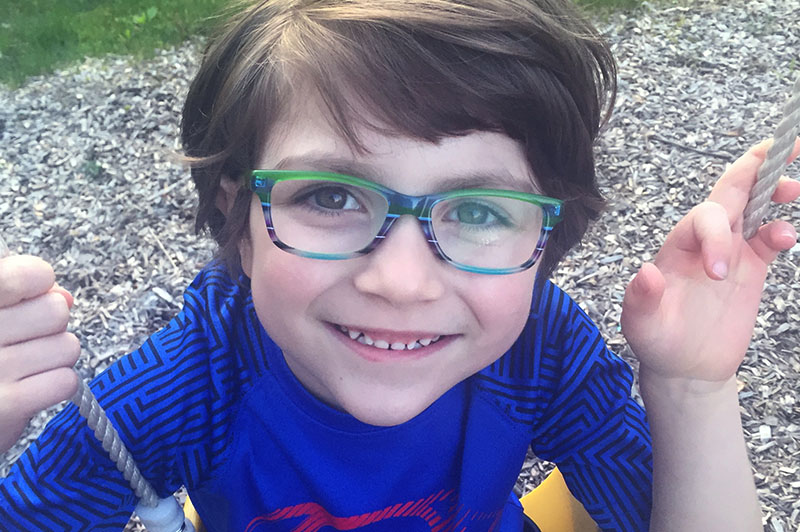
Watch: Understanding a vascular ring reoperation
Boston Children’s Vascular Ring and Airway Program has extensive experience understanding what causes recurring symptoms and determining whether a child needs a vascular ring reoperation or care for another condition.