A heart valve that grows along with a child could reduce invasive surgeries
A prosthetic pulmonary valve replacement can expand over time in a child’s anatomy — potentially reducing the number of invasive replacement surgeries.
At the Complex Biventricular Repair Program, we are always looking for new and safe ways to improve patient outcomes. That’s why we are committed to research and innovation that offers insight on a wide range of biventricular repair procedures that aim to restore a child’s ventricular functions.
Our team’s close alignment with the Congenital Heart Valve Program has led to the development of advanced valve repair and replacement techniques, including expandable valve technology. It all starts with better imaging. New techniques in three-dimensional echocardiography help us understand how valves work and how to improve their function. We can enlarge valve leaflets, replace chords, and reinforce support structures to help preserve native valve function.

A prosthetic pulmonary valve replacement can expand over time in a child’s anatomy — potentially reducing the number of invasive replacement surgeries.
Over the past five years, major advances in technology have allowed us to improve surgical planning and show families, in great detail, how we manage treatment. We work closely with Benderson Family Heart Center engineers to create computational 3-D models that help us visualize patient anatomy before surgery so we can have an accurate understanding of how we can best approach biventricular repair in each child.
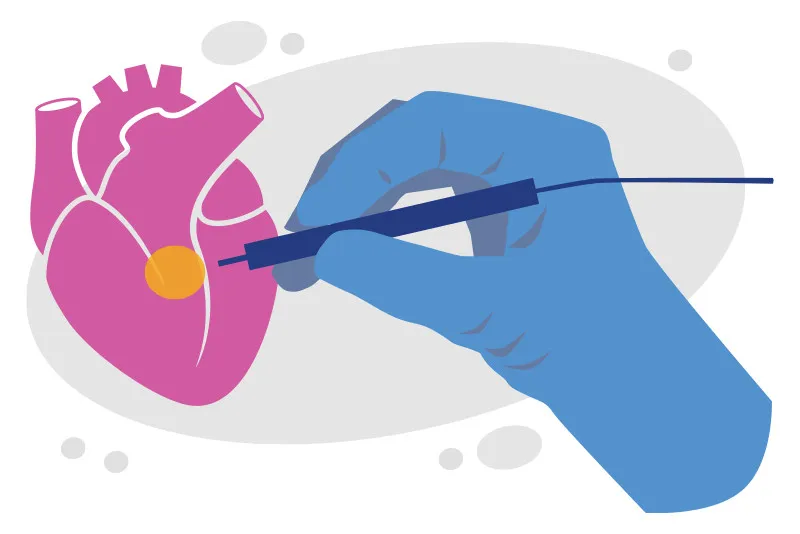
Sitaram Emani, MD, is the principal investigator of this clinical trial, which explores whether injecting mesenchymal precursor cells (MPCs) directly into the left ventricle can help promote growth of the ventricle.
The goal of the trial is to determine if injection of MPCs will improve the chances of those patients with a single ventricle or borderline left ventricle to being converted to biventricular circulation, which could improve their quality of life and longevity over palliation.
During complex biventricular repairs, conduction tissue — the unseen electrical system of the heart — is at risk for injury by a surgical tool, which would prompt the need for a pacemaker. A novel technique, developed by Boston Children’s surgeons and electrophysiologists in our Surgical Electrophysiology Program, identifies conduction tissue during surgery to help us mark where it is and avoid injury.

An electrophysiology tool guides biventricular repair and other surgeries.

How conduction tissue mapping is reducing heart block
Our cardiac surgeons also found that using confocal microscopy could help reduce arrhythmia in congenital heart defect operations.