Pain and the Brain
Neuroimaging studies indicate that pain can activate a wide network of brain areas. These brain regions may reflect activation of different functional networks all relating to different aspects and consequences of pain. Such functions could include not only sensory processing of pain, but also attention-orienting, threat assessment, planning an immediate reaction to resolve pain, and assessing the meaning of the sensation.
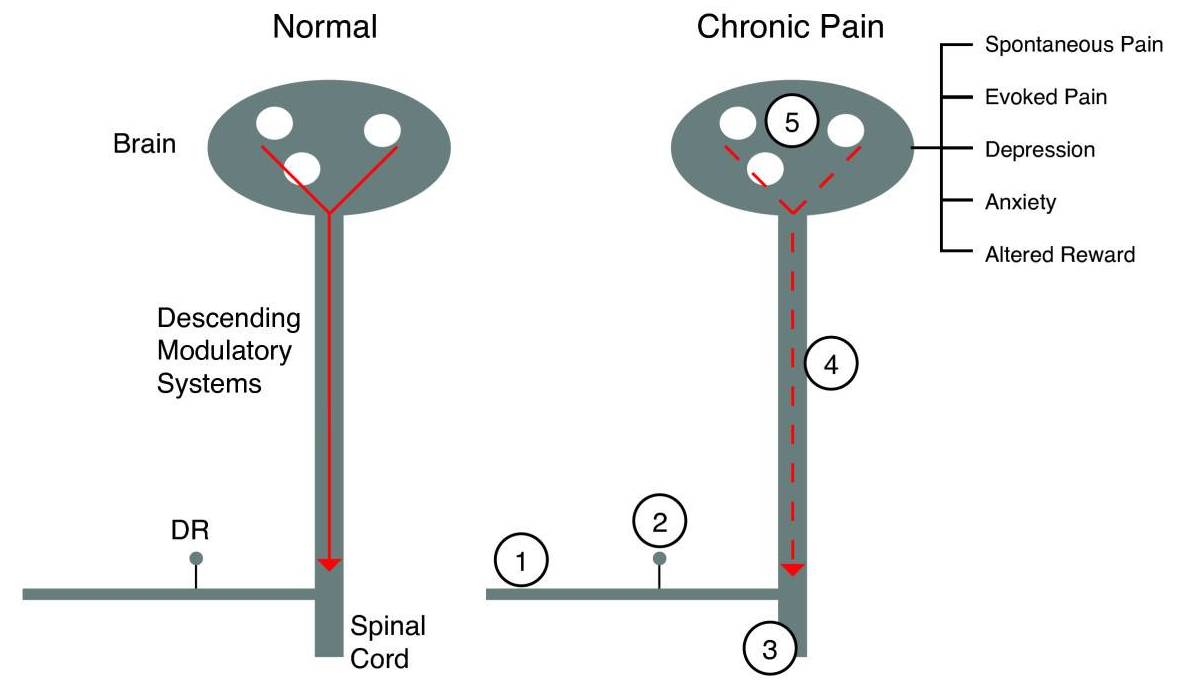
Image from: Borsook, Moulton, Schmidt, and Becerra. Neuroimaging revolutionizes therapeutic approaches to chronic pain. Molecular Pain 2007 3:25 doi:10.1186/1744-8069-3-25. Panel A reprinted with permission from Casey and Tran, 2006.
Pain Neural Networks
Information processing is carried by neural circuits. Defining these circuits using non-invasive neuroimaging in humans and animals allows us to define circuits involved in pain processing. Pain is critical to living organism's adaptation to the environment, which under normal circumstances allows for protection (withdrawal or guarding) of the individual or body part from harm. Much of the information of pain neural circuits has been derived from marine and non-human primate basic science in anatomy, physiology and molecular biology. Clinical work has also contributed to our understanding of these circuits. However, with the advent of non-invasive neuroimaging we can being to dissect, with great clarity and anatomical definition, functional systems within the human brain that are involved in pain processing in healthy volunteers, surrogate models of pain and in patients with acute or chronic pain. For example, our group has been among the first to evaluate the nucleus accumbens and cerebellum in pain in humans. The definition of these circuits also allows us to define specific informational processing systems common to the animal and human, thus allowing specific interrogation of targets for future therapies for chronic pain.
Disease State
While an understanding of neural circuits in healthy volunteers provide insight into normal circuits, understanding the dynamic changes occurring in patients with chronic pain is a bigger challenge. These changes may involve the sensory experience itself (e.g., the development of burning pain or allodynia). The changes may also involve systems involved in the emotional experience in pain such as unpleasantness, depression, or suffering. The use of imaging techniques to identify pain-activated areas in humans that may provide opportunities to follow the effectiveness of new therapeutic approaches, and the information may improve the diagnosis and initiate novel treatment strategies for pain. Objective indices of brain function will provide a targeted method for the evaluation of analgesics in these patients and also objective diagnosis and ability to follow the progression of the disease. Prediction of chronic pain, for example, following surgery may indeed be possible. Such evaluation with imaging techniques include functional (e.g., fMRI), anatomical (e.g., MRI for cortical thickness), and chemical (e.g., spectroscopy).
Clinical Application
Biomarkers for pain are needed in a number of domains. The first is to objectively define pain in humans and animals. The second is to define models that clearly form the basis of altered function in the clinical condition of chronic pain such as neuropathic pain. While the understanding of altered function including neurochemical and structural changes in neurons is beginning to be well understood, in general, the specific understanding of these changes in inflammatory and neuropathic pain are less well understood. Such changes are essential to the understanding of the underlying mechanisms of plasticity of genes that impact on cellular, molecular and physiological changes in pain processing. One approach to surrogate markers is to define specific neural circuits that are seen in the human condition and apply them to experimental human and animal systems. In both, the idea is that activation within a specific readout (surrogate) or neural pathway parallels the clinical condition. Defining objective markers for the evaluation of pain for use in the clinic is part of the overall focus of the program.
Imaging and Analysis
Brain imaging allows for the interrogation of CNS circuits affected by analgesics. Analgesia is defined as loss of pain without loss of consciousness. At the present time, there are no objective methods for defining analgesia. The use of imaging in understanding the functional effects on brain circuitry may significantly contribute to drug discovery and development by understanding how specific chemical agents/entities affect specific CNS circuits involved in pain and analgesia.