Making the Ross procedure a safe aortic valve replacement option
Learn how the Ross procedure gives children a long-lasting aortic valve replacement.
The aortic valve, one of the heart’s four vital valves, plays a critical role in ensuring blood flows properly from the heart to the rest of the body. The valve is nestled within the aortic root, a structure that connects the heart to the circulation system. The aortic valve works in harmony with the aorta (the heart’s main artery to the body) and the left ventricle, which is the primary pumping chamber of the heart. It has three leaflets (also known as flaps or cusps) that control blood flow by opening and closing.
The aortic valve is like a one-way gate that controls blood flow in the right direction. When the heart beats, the aortic valve opens to let blood out of the heart and into the aorta, which carries blood to the rest of the body. Then the valve closes to prevent blood from flowing back into the heart.
Aortic valve disease disrupts this intricate blood flow process, and can cause fatigue, shortness of breath, and potentially heart failure. Many of our patients are born with primary congenital aortic valve disease, which can manifest as a unicuspid (having only one valve flap instead of three) or bicuspid (two valve flaps) condition. Other patients develop a form of the disease after birth.
The disease can present in one of two ways:
The disease and its presentations can also be associated with:
The Congenital Heart Valve Program at Boston Children’s specializes in the care and treatment of aortic valve disease — including offering innovative surgeries such as the Ross procedure and the partial heart transplant.

Learn how the Ross procedure gives children a long-lasting aortic valve replacement.
Our team carefully considers two primary approaches before treating aortic valve disease: aortic valve repair and aortic valve replacement. Our approach depends on the individual case, taking into account a patient’s condition, the severity of the disease, their heart anatomy, and overall health. Using innovative three-dimensional modeling — as well as two- and three-dimensional cardiac echocardiography, CT scans, and cardiac magnetic resonance imaging (MRI) — we can see all aspects of a patient’s aortic valve disease and their heart anatomy, allowing us to determine the right approach for treatment and how we can best preserve the native tissue.
Thanks to advancements in cardiac imaging, we can evaluate the characteristics of a fetus’ heart anatomy. We work closely with the Fetal Cardiology Program to detect and diagnose aortic valve disease and any CHD in the fetal stage. We can potentially intervene before birth with specialized in utero treatment, including procedures such as fetal cardiac intervention and fetal therapy treatments with medications. Working with our colleagues in the Neonatal Cardiac Surgery Program, we also treat newborns for valve conditions such as aortic valve stenosis.
We believe children benefit when their heart valves can be repaired, rather than replaced. We focus on developing solutions and techniques to repair aortic valves so they can remain structurally intact and keep the other parts of the heart strong and healthy. That includes new reconstruction techniques that can improve the function of diseased aortic valves that were once considered untreatable. Here are four types of repair and reconstruction procedures we perform:
Unfortunately, some children have advanced aortic valve disease and repairs aren’t enough. They instead need a replacement valve. This approach involves removing the damaged aortic valve and replacing it with a mechanical or biological valve — or in certain cases, we replace it with a patient’s own pulmonary valve. Mechanical replacement valves are durable but have drawbacks (see below). Also, small prosthetic valves are limited in availability, which means young patients may need more interventions as they grow. We are always trying to extend the life of a replacement aortic valve and avoid the disadvantages of bioprosthetic and mechanical replacement options. Here are four types of aortic valve replacement procedures we perform:
Bioprosthetic tissue that replaces an aortic valve is made from animal tissue (pig or cow). A drawback is the animal tissue might not last long and a patient will eventually need another replacement valve.
These are tissue valves from a human donor. It is commonly used to treat endocarditis (when bacteria infects the heart valve). The benefit is a patient won’t need blood thinners throughout a lifetime, but, similar to bioprosthetic valves, these wear out and eventually need to be replaced.
Mechanical aortic valves are made of strong, durable materials like metal or carbon. They don’t wear out easily and can last a long time. However, the risk of blood clot formation is high, so a patient will have to take blood thinners over a lifetime.
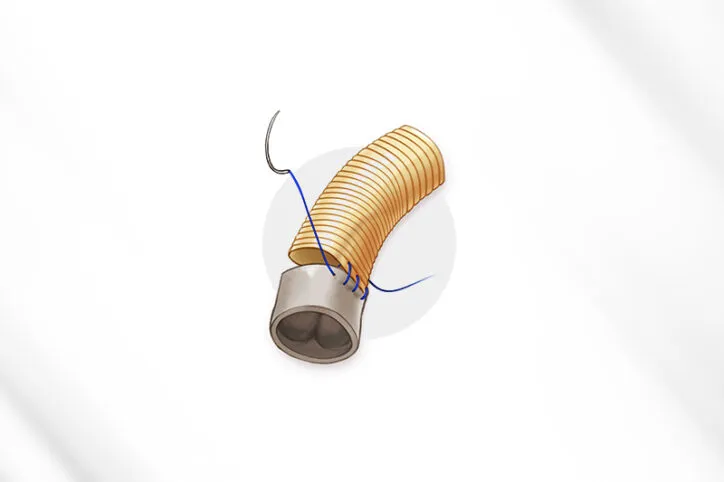
We move the patient’s own pulmonary valve (the valve that controls blood flow from the heart to the lungs) into the place of the damaged aortic valve, which is removed. We then place a donor valve, or conduit, where the pulmonary valve used to be. The advantage of the procedure is that it does not require a patient to take anticoagulation medications throughout their lifetime. A disadvantage is the donated pulmonary valve will probably have to be replaced once or a few times over a lifetime.
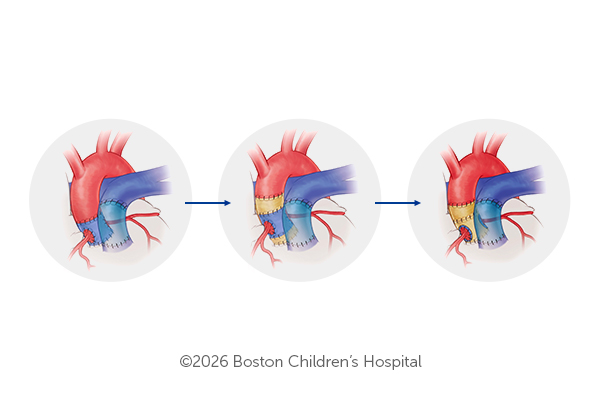
Boston Children’s cardiac surgeons work to ensure a patient’s pulmonary valve can withstand arterial pressure in its new role as an aortic valve. If the valve passes an in-surgery pressurization test — a technique they developed — they then take steps to make it durable and prevent aortic root dilation and blood flow regurgitation, as seen in a series of three illustrations. First, they perform the “inclusion” technique: implanting the valve within the aortic root. Then, they wrap the valve with prosthetic material. They can also take a third reinforcement measure: placing a supportive prosthetic ring around the aorta.
To reduce replacement procedures, our team developed a unique surgical technique that aims to prevent complications such as aortic root dilation (an abnormal widening of the aortic root) and blood flow regurgitation. We pressurize the pulmonary valve during surgery as a test to see if it will withstand increased blood pressure as an aortic valve. If it passes the test, we support the new aortic valve with prosthetic wrapping to keep it durable and potentially last long.
Learn how our cardiac surgeons developed an in-surgery pressurization test to prevent complications and make a new aortic valve durable.
In 2024, our heart specialists started offering another aortic valve replacement option: transplanting a donor’s healthy valve into a patient’s heart. Because it is human tissue, the donated valve should require a lesser amount of immunosuppressives for several months after the procedure. But just as importantly, the valve should grow along with the patient’s heart anatomy.

Our cardiac surgeons performed a partial heart transplant on 4-year-old Jack. It’s possibly the first such transplant as an elective procedure, and probably the first of many at Boston Children’s.