Bladder Exstrophy | Symptoms & Causes
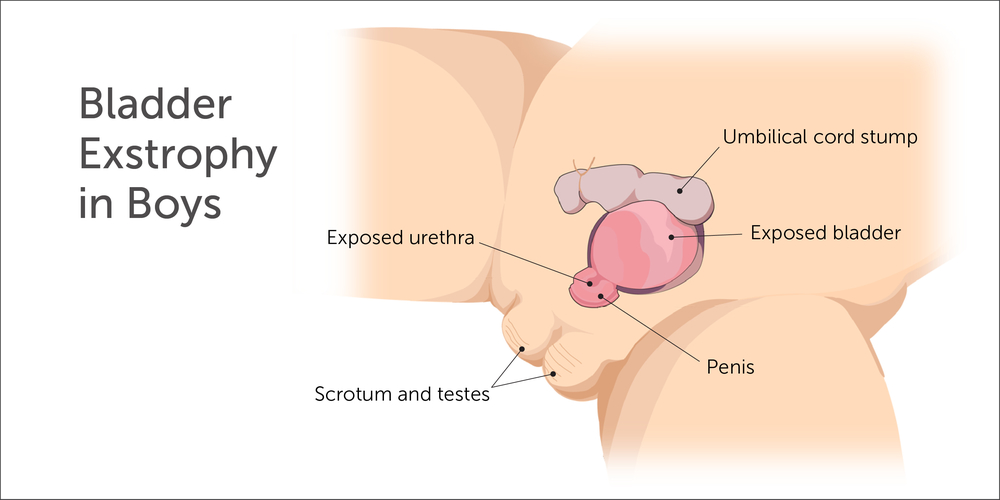
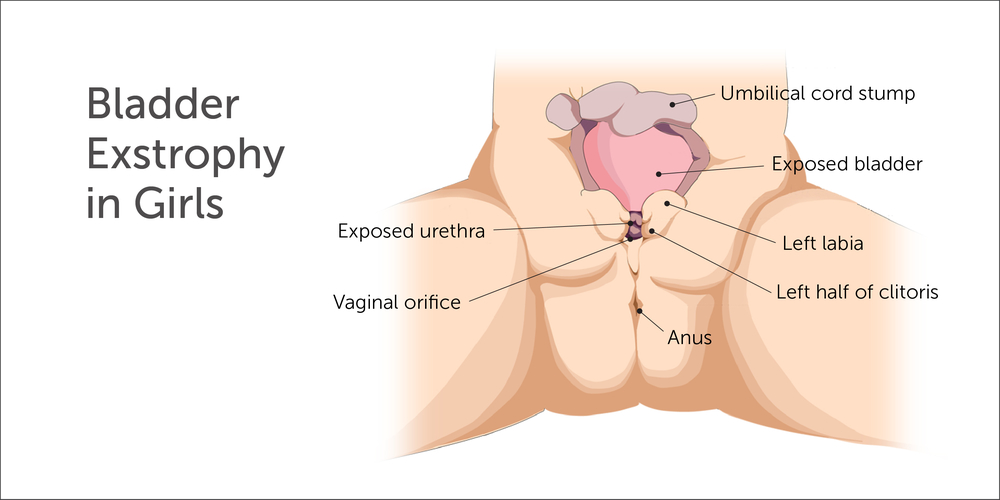
What causes bladder exstrophy?
The exact cause of bladder exstrophy is unknown. Popular theories suggest a normal structure known as the cloacal membrane may not develop normally. This may prevent appropriate tissue development, ingrowth, and the joining together of the supportive lower abdominal wall structure. It is very unlikely that parents will have more than one child with bladder exstrophy.
Bladder Exstrophy | Diagnosis & Treatments
How is bladder exstrophy diagnosed?
Bladder exstrophy may be diagnosed during a routine fetal ultrasound or other imaging techniques such as fetal magnetic resonance imaging (MRI). However, bladder exstrophy is frequently not identified during the prenatal period and diagnosed immediately after birth during the initial physical examination. When bladder exstrophy is diagnosed during the prenatal period, this allows time for families to learn about the condition and prepare for care after delivery.
How is bladder exstrophy treated?
It is important to note that there are typically no emergency medical needs immediately after birth. Following birth, we advise families to seek care from experienced centers that regularly take care of patients with bladder exstrophy. The primary surgical goals when caring for a child with bladder exstrophy are to:
- Close the bladder and place it inside the body
- Provide acceptable appearance and function of the external genitalia
- Ensure your child has a typical childhood
About bladder exstrophy repair
At Boston Children’s, we offer a range of surgical options for treating bladder exstrophy, including the Kelly procedure and complete primary repair of bladder exstrophy (CPRE) — both of which we offer as single-stage repairs. Single-stage repairs may reduce the number of surgeries your child needs, time under anesthesia, and earlier recovery and development.
Our surgeons perform complete primary repair of bladder exstrophy with the Kelly procedure (also known as Radical Soft Tissue Mobilization) in boys and girls. This operation is performed in a single stage procedure, meaning that bladder closure, bladder neck reconstruction, urethral repair, and genital reconstruction are all done during one surgery.
For girls, our surgeons typically perform CPRE, where the bladder is closed, the bladder neck (area of transition from bladder to urethra) is reconstructed, and the epispadias is repaired (entire urethra is closed into a tube) at the same time.
The ureters, which connect the kidneys to the bladder, may be reimplanted to help prevent vesicoureteral reflux (VUR). Children may require additional surgery during later years to manage urinary incontinence and urinary tract infection.
The day prior to complete primary repair, your baby undergoes osteotomies by an orthopedic surgeon, and an epidural catheter is placed to help with pain related to the operation. The osteotomies allow for a safe reconstruction the following day by taking the tension off the bladder and abdominal wall. By separating the osteotomies and surgical reconstruction of the bladder, we have been able to avoid intensive care unit admissions following our surgical reconstruction. After the osteotomies, your baby is fit for a spica cast, which remains in place approximately eight weeks after CPRE to optimize safety and healing. Our average length of stay in the hospital is approximately seven to 10 days after the surgery.
Single-staged surgical approaches such as the Kelly procedure and CPRE are typically performed eight to 12 weeks after a patient is born. This timing presents an opportunity for normal bonding between the baby and parents before the initial reconstructive surgery and lengthy recovery period that follows. The time between birth and initial repair allows for growth, development, and additional maturation of some organs and systems prior to the complex surgery and makes the anesthesia and surgery safer.
Other centers may prefer a staged approach to bladder exstrophy care, where the bladder closure, bladder neck reconstruction, and epispadias repair are divided into separate time points. At Boston Children’s Bladder Exstrophy Program, we have experience in repairing bladder exstrophy in stages. There is a possibility that your child’s anatomy may make a staged reconstruction the preferred surgical approach.
What is the long-term outlook for bladder exstrophy?
After initial treatment for bladder exstrophy, your child will require lifelong follow-up. Care is ongoing and can involve a range of testing to evaluate your child’s growth and development, urinary continence, kidney function, and sexual and reproductive health. In many instances, behavioral modification, medications, and physical therapy are incorporated as part of the post-surgical treatment plan. In some cases, additional surgery may be required during childhood, adolescence, and young adulthood.
Boston Children’s is committed to providing the care that your child needs. Every child is different, and, as your child grows, their bladder and kidneys grow with them. Our team in the Bladder Exstrophy Program will work with you to develop the best plan of care specific to your child’s needs.
How we care for bladder exstrophy
The experts in our Bladder Exstrophy Program provide exceptional pediatric care. Our team includes physician specialists in urology, nephrology, orthopedic surgery, anesthesiology, radiology, and nuclear medicine, as well as nurses, social workers, and child life specialists who will care and support you and your child at every step, from diagnosis through treatment, and even after your child returns home. We are always here to answer any questions and to listen to your concerns.
We offer a variety of resources for families, including access to the Fetal Care and Surgery Center (FCSC). The FCSC provides support through prenatal counseling, treatment, and follow-up for families with a confirmed or suspected fetal congenital anomaly. In addition, medical staff, social workers, child life specialists, and spiritual care services are available to support expectant parents.