Less oxygen-rich blood is pumped throughout the body because the hole between the left and right atria diminishes blood flow to the left ventricle, the main pumping chamber. The right ventricle ends up working harder and can weaken because it is now pumping oxygen-poor and oxygen-rich blood.
Breadcrumb
- Home
- Conditions & Treatments
- Atrial Septal Defect
What is an atrial septal defect (ASD)?
An atrial septal defect (ASD) is a hole in the middle of the heart wall (septum) that separates the upper-right and upper-left chambers (atria) of the heart. It causes oxygen-rich blood and oxygen-poor blood to mix, which can lead to problems such as high blood pressure or an increased risk of stroke.
Atrial septal defects in children and adults may need treatment if they are large or cause poor health. Most atrial septal defects can be treated with a nonsurgical approach called cardiac catheterization, but some may require surgery. At Boston Children’s Benderson Family Heart Center, our team of specialists is highly skilled in the full range of treatment options, from cardiac catheterization to minimally invasive surgical approaches to full sternotomy. In fact, Boston Children’s is one of just a few pediatric hospitals in the U.S. to offer a minimally invasive procedure called thoracotomy to adults and children with atrial septal defects.
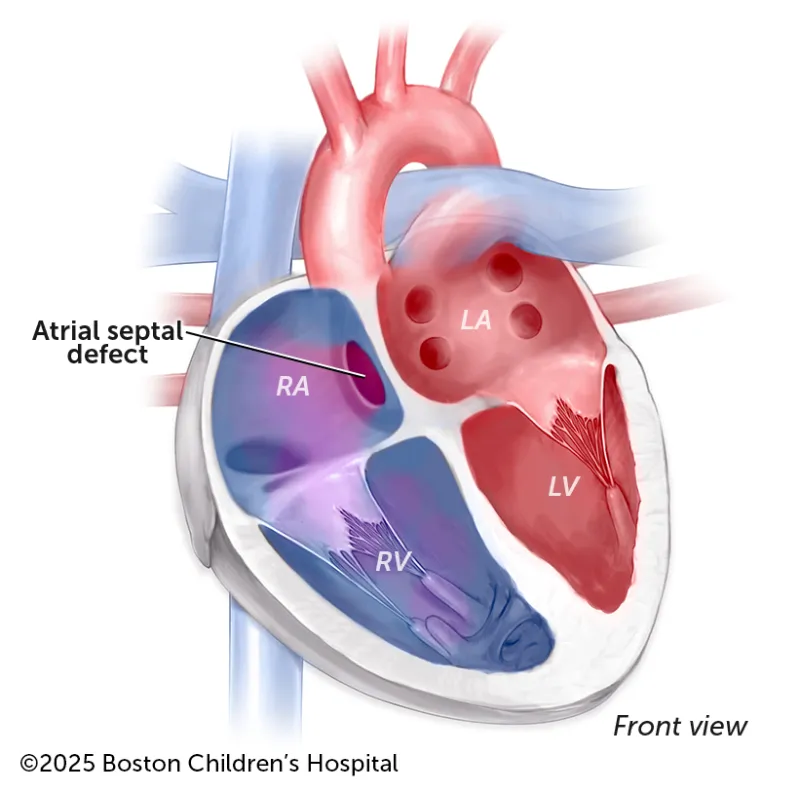
LA: Left atrium
How does an atrial septal defect affect heart function?
An atrial septal defect on its own or in combination with other congenital heart defects (CHDs), such as hypoplastic left-heart syndrome (HLHS), can cause the right side of the heart to enlarge from working too hard. A child who has an atrial septal defect coupled with high blood pressure in the lungs or the CHD tetralogy of Fallot can experience a decrease in blood saturation levels.
Symptoms & Causes
What are the symptoms of an atrial septal defect?
Pediatric atrial septal defects don’t typically cause symptoms until a child reaches school age. However, children who are born prematurely or who have other CHDs, such as mitral valve disease, may experience symptoms of an atrial septal defect as early as birth.
Symptoms can include:
- Rapid breathing
- Decreased endurance
- Slow weight gain and growth
- Frequent respiratory infections
Diagnosis & Treatments
How is an atrial septal defect diagnosed?
Although pediatricians can detect atrial septal defects in children by hearing a heart murmur during a checkup, sometimes the condition is not diagnosed for many years. In fact, atrial septal defects go undetected so often that they are the most common CHD diagnosed in adulthood. Depending on the type of heart murmur your doctor hears, they may recommend one or more or the following tests:
- Echocardiogram (cardiac ultrasound)
- Electrocardiogram (ECG)
What are the treatment options for an atrial septal defect?
Some atrial septal defects can close on their own, usually before age 3. However, if the defect remains and a significant amount of blood is passing through the hole, it may need to be treated. At Boston Children’s, we offer a spectrum of treatment options to close atrial septal defects in children and adults. Your child’s care team will work with your family to help determine the best treatment approach.
Cardiac catheterization
Most atrial septal defects can be safely closed with a nonsurgical approach called cardiac catheterization. During this procedure, the doctor will insert a long thin tube (a catheter) that leads a small umbrella-shaped closure device through a leg vein. The catheter will guide the closure device to the heart, where the device will open to cover the ASD with a patch.
Your child will be given deep sedation or general anesthesia before the procedure and should feel little to no discomfort. They typically go home the day of the catheterization.
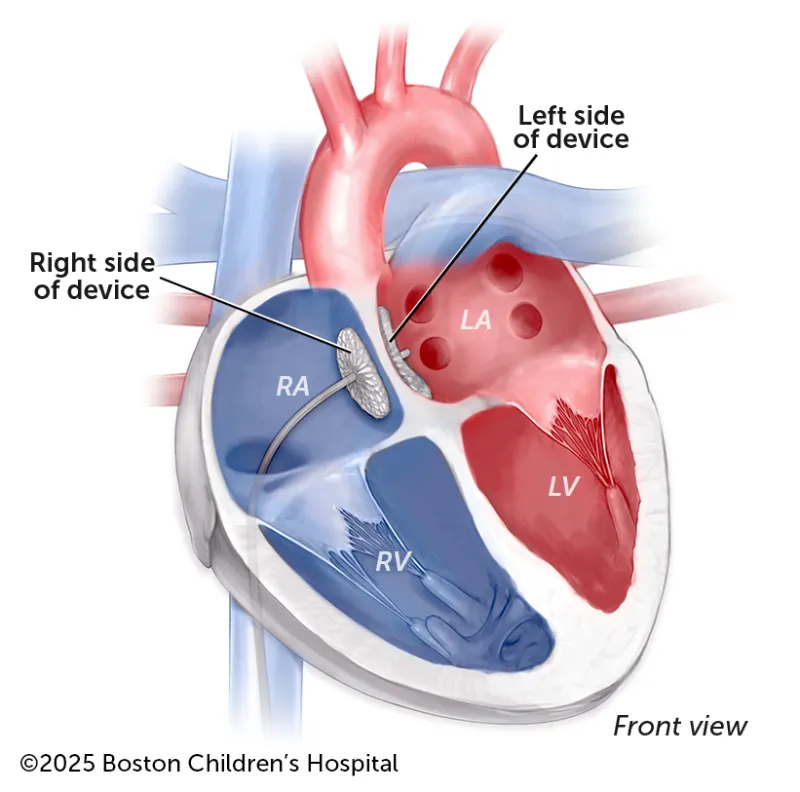
Cardiac catheterization patches the hole caused by an atrial septal defect and enables the heart to pump blood normally: the left side pumping only oxygen-rich blood and the right side pumping only oxygen-poor blood.
Surgical approaches
If catheterization cannot close your child’s atrial septal defect, we will recommend open-heart surgery to place a patch over the hole. Most hospitals repair an atrial septal defect with a sternotomy, in which surgeons access the heart through the sternum (breastbone). The procedure leaves a visible scar on the upper chest and the sternum must be wired together to help the bone heal. Sometimes the thymus gland must be removed to give surgeons a complete view of the heart. Recovery in the hospital after a sternotomy can last four to five days, and it can take three months for the sternum to heal.
At Boston Children’s, we also offer two minimally invasive cardiac surgery approaches that avoid certain aspects of a sternotomy for eligible patients:
Thoracotomy
Boston Children’s is one of just a few pediatric hospitals to offer this approach to closing atrial septal defects in children and adults. During a thoracotomy, our surgeons make an incision under the armpit, keeping their sternum intact and leaving a relatively smaller incision scar. The thymus also doesn’t need to be removed. Your child will experience less pain than they would after a sternotomy, and their recovery time in the hospital will be shorter: possibly two to three days. With a faster recovery, they’ll be able to resume physical activities and contact sports as soon as possible after surgery.
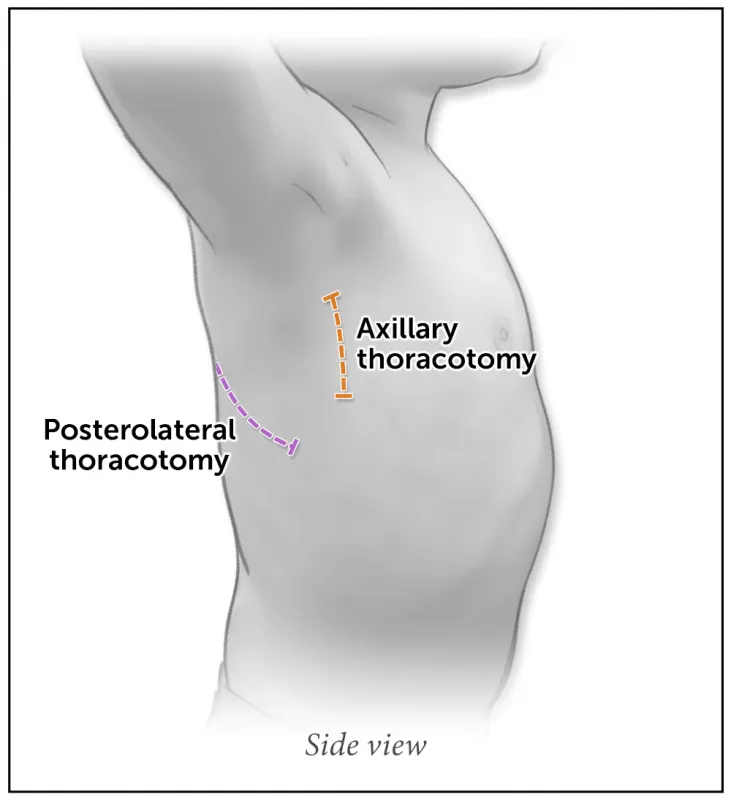
The axillary and posterolateral are two ways to perform a minimally invasive thoracotomy and repair an ASD.
Mini-sternotomy
If your child is not eligible for a thoracotomy, they might be a candidate for a mini-sternotomy. This approach requires a smaller incision to the sternum, either the upper or lower portion. It leaves a small scar on the chest, and your child should feel less pain after surgery. They could leave the hospital within two to three days and should recover within a month.
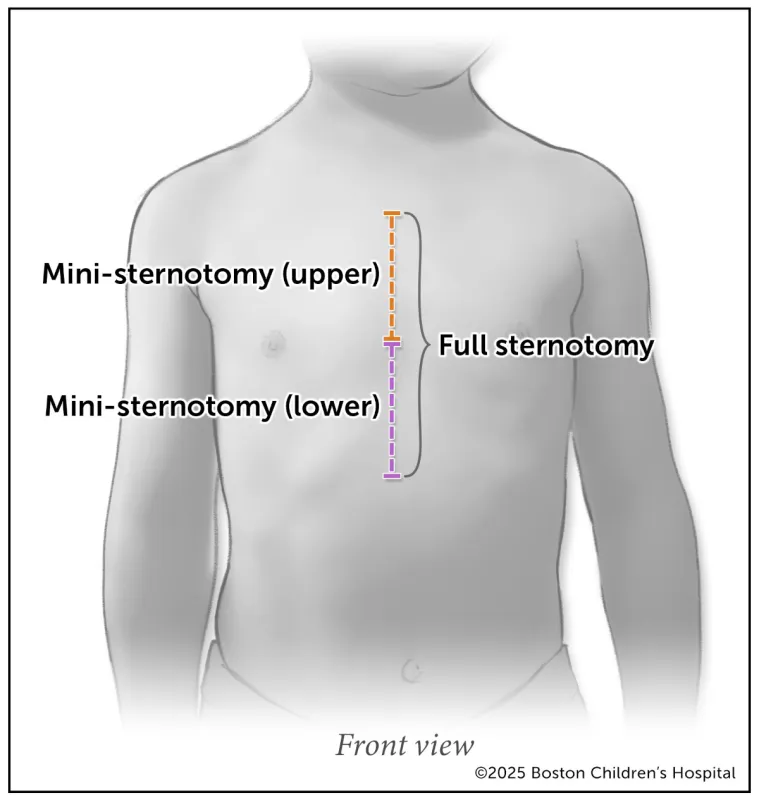
Whereas a full sternotomy splits the entire breastbone, a mini-sternotomy makes a smaller incision, on either the upper or lower portion of the sternum.
Cardiac Conversations: Minimally invasive ASD repair
In this webinar, Boston Children’s heart specialists explain surgical options for ASD repair and how their team strives to improve patient recovery.
Supporting your family through recovery and beyond
Our specialists have extensive experience treating atrial septal defects and will review all treatment options with your family. No matter what your decision is, your family will have all the time and resources you need to think it over, and we are always available to answer any questions.
Working with the Enhanced Recovery After Cardiac Surgery (or ERAS Cardiac) Program, our team will always focus on maximizing safety, minimizing pain, and shortening your child’s length of stay at the hospital and their overall recovery. And once your child is home, our team will continue to follow their progress and heart health into adulthood.

