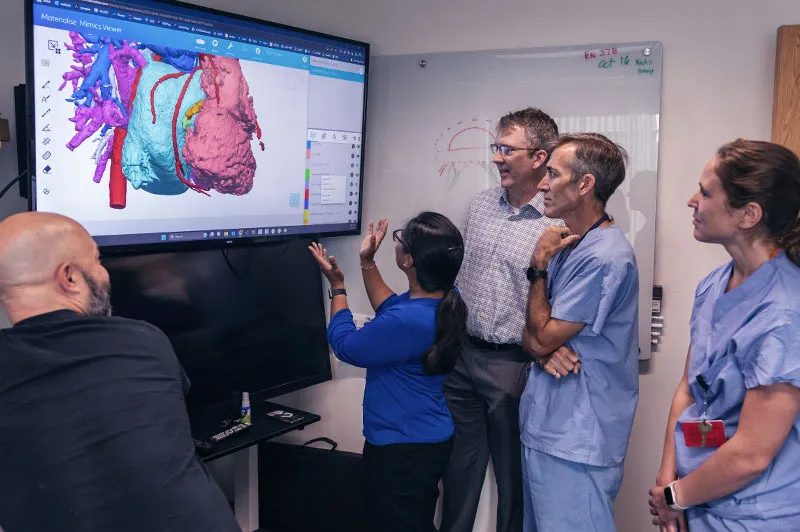
Learn how 3D modeling has transformed the planning of surgery by showing details of a patient’s heart.
Breadcrumb
- Home
- Conditions & Treatments
- Truncal Valve Disease
What is a truncal valve?
When a child has only one main blood vessel attached to the heart, instead of two, it creates one large valve, a truncal valve. The condition, which is a congenital heart defect (CHD), is known as truncus arteriosus. A newborn with this condition can develop truncal valve disease (truncal valve stenosis, truncal valve regurgitation).
How does truncal valve disease affect circulation?
Typically, the pulmonary artery delivers oxygen-poor blood to the lungs, while the aorta (the heart’s main artery) distributes oxygenated blood to the body’s circulatory system. But truncus arteriosus prevents those two arteries from separating in the prenatal development stage. It instead causes the creation of just the one large truncal valve, which will do the work of two valves, the aortic valve and pulmonary valve.
Without a proper pulmonary valve, oxygen-rich (red) blood and oxygen-poor (blue) blood mixes and flows through the lungs and body. Further affecting a child’s health is how the truncal valve is positioned over the left and right ventricles, and the wall that typically separates those two chambers has a hole. This is a condition known as ventricular septal defect (VSD). It sends extra blood to the lungs and makes them work harder. The increased runoff of blood is truncal valve disease. The condition is also associated with the anomalies, or differences, that surface during the fetal development of the heart’s coronary arteries.
Children with truncus arteriosus and truncal valve disease can be fatigued, experience shortness of breath and a rapid heart rate, experience curbed physical development, and face the potential of heart failure.
Diagnosis & Treatments
Treatment for truncal valve disease starts with fetal care
A child who has truncal valve disease will need a lifetime of care. The Congenital Heart Valve Program at Boston Children’s specializes in the care and treatment of truncal valve disease. That care often starts at birth. Using two- and three-dimensional cardiac echocardiography, CT scans, and cardiac magnetic resonance imaging (MRI), we work closely with the Fetal Cardiology Program to detect and diagnose truncal valve disease and any CHD in the fetal stage. We can potentially intervene before birth with specialized in utero treatment. We are at the forefront of fetal cardiac care and have performed more than 185 interventions.
How we approach treatment for truncal valve disease after birth
Getting that head start on care also allows us to treat a child immediately after birth. We work closely with Boston Children’s Neonatal Cardiac Surgery team to ensure treatment planning starts as soon as possible. A few weeks after a child is born and is ready for surgery, we separate the truncus arteriosus into two proper arteries, the pulmonary and aorta. We also repair the VSD.
Most truncal valves are repaired without having to replace it. That’s because when we separate the truncal valve, we use surgical techniques for an aortic valve repair, to ensure that what becomes a new aortic valve properly functions. Those techniques are:
- Simple leaflet repair: This procedure focuses on restoring an existing damaged leaflet of the aortic valve by thinning or implanting it again.
- Complex leaflet repair/bicuspidization: This involves more intricate modifications of the valve leaflets and their relation to the aortic root and neighboring aorta. The bicuspidization technique creates two symmetric leaflets.
- Valve-sparing aortic root repair: This procedure preserves the native aortic valve and replaces the aortic root, which is the section of the aorta connected to the heart. For some patients, the diseased aortic valve cannot be repaired and must instead be replaced with a mechanical or biological valve.
- Ozaki procedure: Also known as neocuspidization, the Ozaki procedure is a complex aortic valve treatment that reconstructs degenerated leaflets. We create customized leaflets from a patient’s own tissue (pericardium). During the same surgery, we create a functioning pulmonary vessel by implanting a homograft (human tissue valves) or artificial conduits (tubes). We also close the VSD with a patch to separate the two lower ventricles.
Because truncal valve disease is associated with abnormalities and malformations of the coronary arteries, we also work closely with the Coronary Artery Program to treat those coronary arteries.
We also perform truncal valve repairs for older patients who didn’t have treatment earlier in life and now experience valve stenosis and regurgitation.