Osteochondritis Dissecans | Symptoms & Causes
What are the symptoms of osteochondritis dissecans?
The first sign of an osteochondritis dissecans injury may be a “popping” sensation in the injured joint. Most people can still use the injured joint, and unfortunately many athletes keep playing, which often makes the injury worse.
When symptoms of inflammation set in, the affected joint feels painful and tight. Your child may also have:
- soreness or tenderness at the joint
- swelling or stiffness around the joint
- difficulty fully straightening the arm or leg
- feeling like the joint is locking, “catching,” or “giving way”
- collection of fluid around the joint (“water on the knee”)
The signs and symptoms of osteochondritis dissecans can resemble those of other overuse injuries. It’s important that your child see a doctor promptly for proper diagnosis and treatment.
What causes osteochondritis dissecans?
Young athletes involved in high-impact sports can sustain an osteochondritis dissecans injury from motions that put repetitive stress on the joint.

Meet Grady
He was playing hockey at the highest level a 12-year-old player in Canada could play when osteochondritis dissecans in both knees forced him to take time off. Three years later, he was drafted by a team in the Ontario Hockey League.
Osteochondritis Dissecans | Diagnosis & Treatments
How is osteochondritis dissecans diagnosed?
To diagnose osteochondritis dissecans, an orthopedic specialist will take a medical history and perform a physical exam on your child. The doctor will check for pain along the affected joint line and may order an x-ray or MRI to help them see the joint.
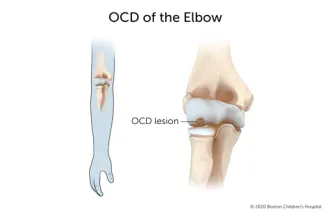
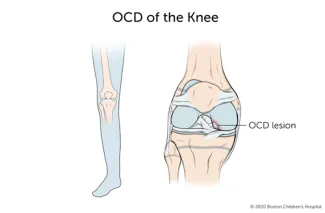
Diagnosing OCD of the knee, elbow, and ankle
To diagnose osteochondritis dissecans, your child’s doctor will assess the affected joint for any swelling or tenderness. They will also test the range of motion of the joint. This may include specialized manipulations of the joint, such as a Wilson test of the knee, to see if a particular rotation of the knee causes pain. To diagnose osteochondritis dissecans of the elbow, ankle or another joint, your child’s doctor will perform similar specialized manipulations.
Testing for osteochondritis dissecans
Various tests may be used to confirm the osteochondritis dissecans diagnosis.
- X-rays: Typically, multiple x-ray views are taken to confirm and assess the extent of the injury. X-rays may also be taken of the same joint on the other limb as a basis for comparison.
- MRI (magnetic resonance imaging): An MRI can show whether the loose piece is still in place or has moved into the joint space.
How is osteochondritis dissecans treated?
Your child may not need surgery if the loose piece of bone has not detached. They will need to take a break from high-impact sports while they heal. Their physician may recommend rest, ice, compression, and elevation (RICE), combined with non-steroidal anti-inflammatory medications for pain.
Surgical repair
Your child may need surgery if the OCD lesion is unstable, if a fragment of bone or cartilage has broken off into the joint, or if the injured area does not heal after a course of rest.
Your child’s doctor will select a surgical technique based on the type of osteochondritis dissecans, your child’s age, and other factors. Surgical procedures to repair osteochondritis dissecans of the knee or elbow include:
- drilling small holes in the underlying bone to stimulate healing
- removing or securing loose fragments of bone
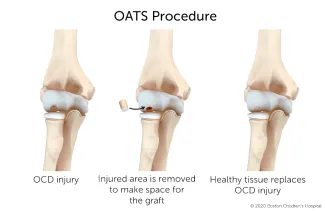
- a procedure called osteochondral autologous transplantation surgery (OATS)
Osteochondral autologous transplantation surgery (OATS)
OATS, or osteochondral autologous transplantation surgery, is a treatment option for certain OCD injuries. The procedure involves replacing injured bone and cartilage in the joint with healthy tissue taken from another part of the body, such as the side of the knee.
What is the long-term outlook for osteochondritis dissecans?
After surgery, your child may need to wear a cast or brace while their joint heals. They may need to complete a course of physical therapy before gradually resuming activity or sports.
Your child should be able to return to sports and activities after their knee, elbow, or other joint has regained strength and stability — usually around six months after surgery. If your child’s joint remains painful or unstable after surgery and a period of recovery, their doctor may recommend lifestyle changes such as switching to low-impact sports.
How we care for osteochondritis dissecans
The Boston Children’s Hospital Orthopedics and Sports Medicine Center provides comprehensive assessment, treatment, and follow-up care to children, adolescents, and young adults with osteochondritis dissecans. We understand the importance of sport in young athlete’s lives and are dedicated to providing the best care possible to help our patients return to their sports safely, without risking further injury.
Members of our orthopedics and sports medicine team travel to local and regional schools, youth groups and sports clubs to teach leg strengthening and other techniques with a goal of dramatically reducing overuse injuries like osteochondritis dissecans. We also conduct safe-training programs and clinics for coaches.
Patient resources
Osteochondritis dissecans of the elbow
This downloadable patient education sheet describes the symptoms, causes, and treatments for osteochondritis dissecans of the elbow.