Guillain-Barre Syndrome | Symptoms & Causes
What are the symptoms of Guillain-Barré syndrome?
Each child may have different symptoms, but some of the most common symptoms include:
- weakness or pain in the legs and arms (usually begins in the legs)
- problems walking
- pain, numbness, or tingling in the toes and fingers
- feeling lightheaded or dizzy
- weakness in the face
- breathing problems (in severe cases)
If your child is having trouble walking, call your primary care provider right away or go to an emergency room.
What are the causes of Guillain-Barré syndrome?
Doctors don’t completely understand the causes of Guillain-Barré. In some cases, it occurs after a mild viral or bacterial infection. Occasionally, it can occur after an immunization. Often, however, there is no known cause.
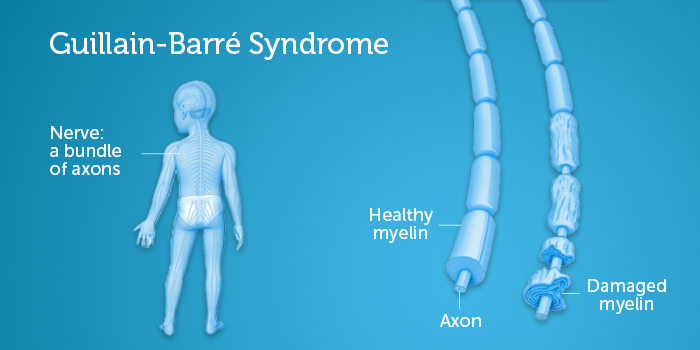
Experts believe that the reason why infections can trigger autoimmune conditions such as Guillain-Barré is that when the immune system attacks the invading viruses or bacteria, it can sometimes also attack healthy tissue.
Although some vaccines have been linked with Guillain-Barré in the past, this is extremely rare. If you have any concerns about vaccines, talk with your child’s pediatrician. You may also find this information from the Centers for Disease Control and Prevention (CDC) helpful.
Guillain-Barre Syndrome | Diagnosis & Treatments
How is Guillain-Barré syndrome diagnosed?
Guillain-Barré is diagnosed based on your child’s symptoms and the results of some specific tests. A pediatrician or pediatric neurologist will examine your child, review his or her medical history, and ask about specific symptoms.
The key to managing Guillain-Barré syndrome is to diagnose it early so your child can get proper care.
What tests will my child need?
There are three tests that the clinician may use to help diagnose Guillain-Barré:
- Lumbar puncture (spinal tap): For this test, a special needle is placed into your child’s spinal canal (the area around the spinal cord) in the lower back, and a small amount of cerebrospinal fluid (CSF) is removed. Doctors test the fluid sample for signs of inflammation.
- Electromyography and nerve conduction studies (EMG testing): These tests measure the electrical activity of nerves and muscles.
- Magnetic resonance imaging (MRI): This test may be used to get a picture of your child’s spine. It’s used less often than lumbar puncture and EMG in diagnosing Guillain-Barré. However, if it’s not possible to do one of the first two tests, doctors make take an MRI of your child’s spine.
These tests are usually done without sedation or anesthesia. In some cases, anesthesia may be needed.
What are the treatment options for Guillain-Barré syndrome?
Your child will probably need to be admitted to the hospital so doctors can watch for complications and help him or her recover.
Guillain-Barré syndrome is very treatable, and most of children recover fully or with only mild long-term weakness. Most children can go home from the hospital within a week.
Immune system treatments
Guillain-Barré syndrome is usually treated with immune system treatments, which help your child's immune system go back to working normally. There are two types:
- Plasma exchange (plasmapheresis) is a procedure that filters your child’s blood though a machine. During plasma exchange, blood is temporarily removed from your child's body to filter out abnormal antibodies. The filtered blood is then returned to his or her body along with albumin or plasma from blood donors.
- Immunoglobulin therapy (IVIG) involves infusing a blood product called immunoglobulin through an IV line into your child's veins. Immunoglobulin is pooled from multiple donors that contain normal antibodies.
Supportive treatments
Depending on your child’s particular condition, he or she may need other tests or treatments while in the hospital.
- If your child's blood pressure is going up and down, the medical team may do an echocardiogram or electrocardiogram (EKG) to check his or her heart.
- If your child is having trouble breathing, he or she may need to be placed on a ventilator (breathing machine) until he or she is able to breathe again.
- Your child may get pain medications to control pain.
How we care for Guillain-Barré syndrome
At Boston Children’s Hospital, specialists in our Neuromuscular Center are experienced diagnosing and treating children of all ages with Guillain-Barré syndrome. Our program brings together pediatric specialists from neurology and other fields to provide comprehensive care for our patients.
We also provide follow-up outpatient care for children recovering from Guillain-Barré through the Department of Physical Therapy and Occupational Therapy Services.