Breadcrumb
- Home
- Conditions & Treatments
- Deep Brain Stimulation
About deep brain stimulation therapy
Boston Children’s Hospital is now offering deep brain stimulation (DBS) for children with primary dystonia, a type of movement disorder in which faulty brain signals cause involuntary muscle contractions. These lead to abnormal, taxing movements, typically repetitive twisting or contorting of the arms, legs, neck, or other body parts. Primary dystonia, unlike secondary dystonia caused by a brain injury, is thought to be genetic in origin.
Dystonia may occur only in a specific part of the body, like the eyelid or hand, or it may affect many body regions. Often, the dystonia progresses and spreads most rapidly in the first five years after its onset, then begins to stabilize. Dystonia may be present at rest, but often becomes much worse when the child is doing a specific task or motion, like writing or walking. As a result, dystonia can become highly disabling.
Primary dystonia is often painful, and the abnormal movements and postures may embarrass the child and make it difficult to perform well in school. Some children become wheelchair-bound, and if dystonia is left untreated for years, it can cause permanent damage to joints and muscles as the limb “freezes” into the dystonic position. Most children with primary dystonia have a normal life expectancy.
What is deep brain stimulation and how can it help?
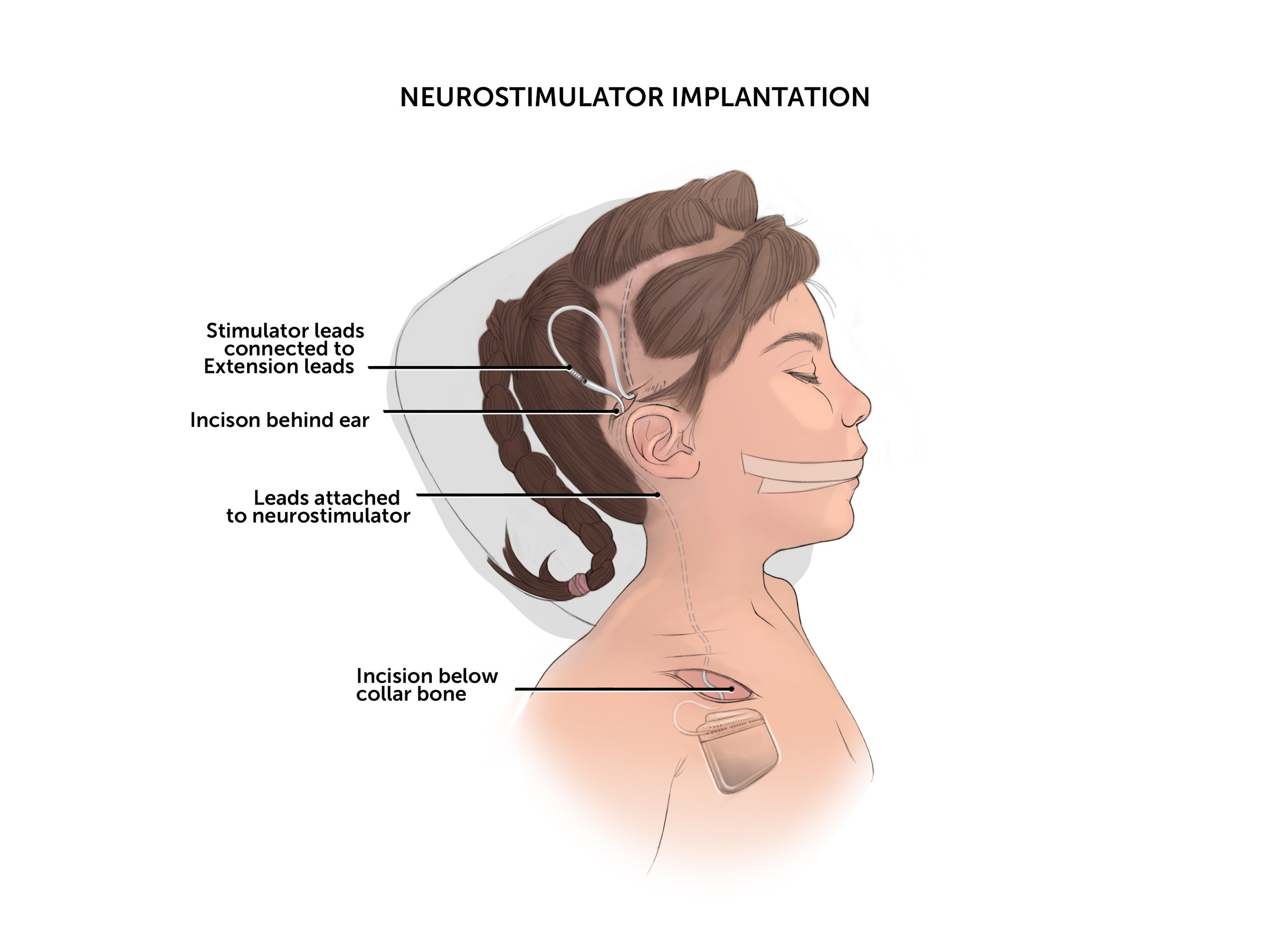
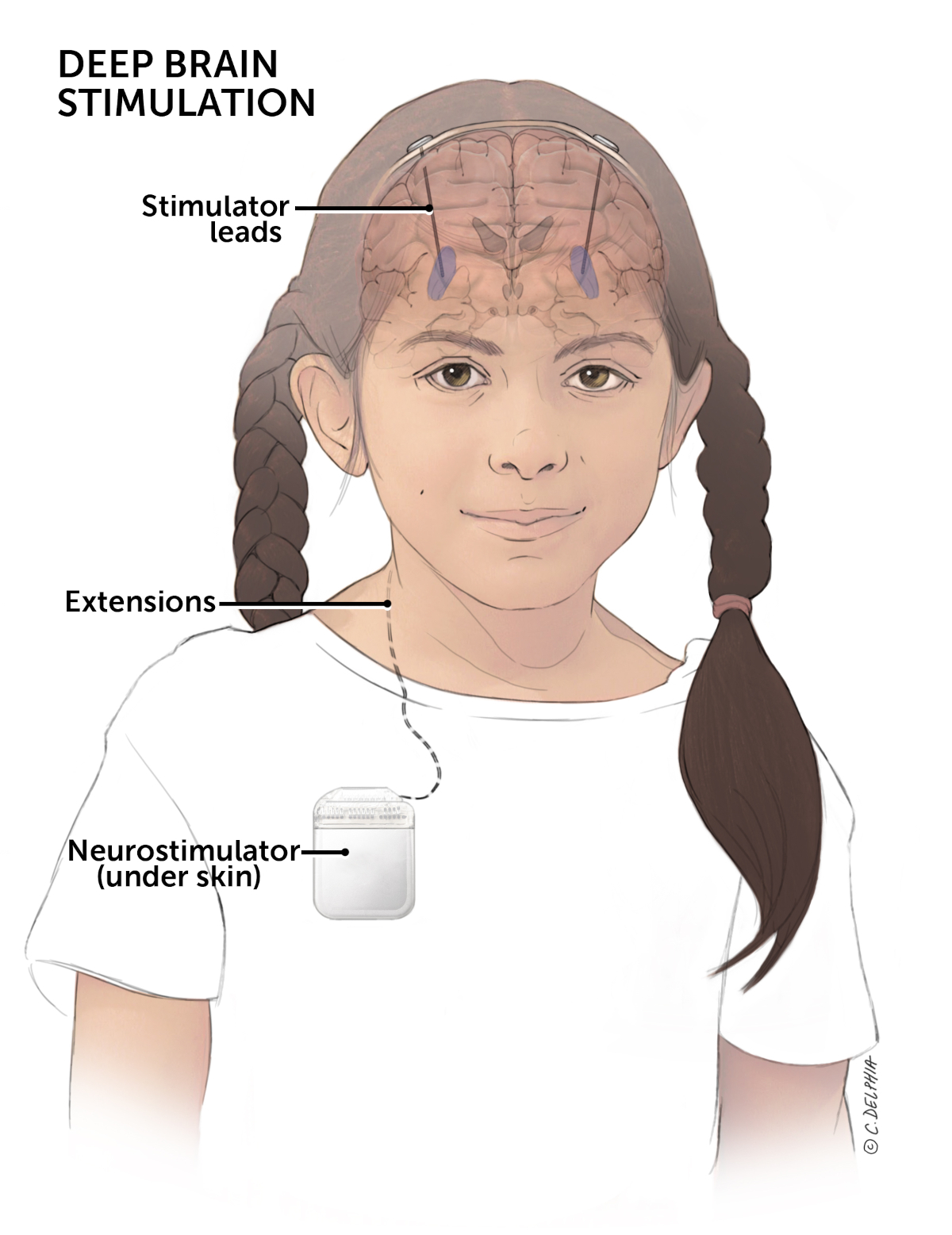
DBS therapy uses a small device similar to a pacemaker, called a neurostimulator, to send mild electrical pulses to the parts of the brain that are responsible for the involuntary movements. The neurostimulator, manufactured by Medtronic, is implanted just under the skin, usually below the collarbone. It is connected to electrodes (or “leads”) implanted in the brain by a thin, flexible wire. The electrodes are precisely placed in a part of the brain called the basal ganglia, part of the brain's motor circuit.
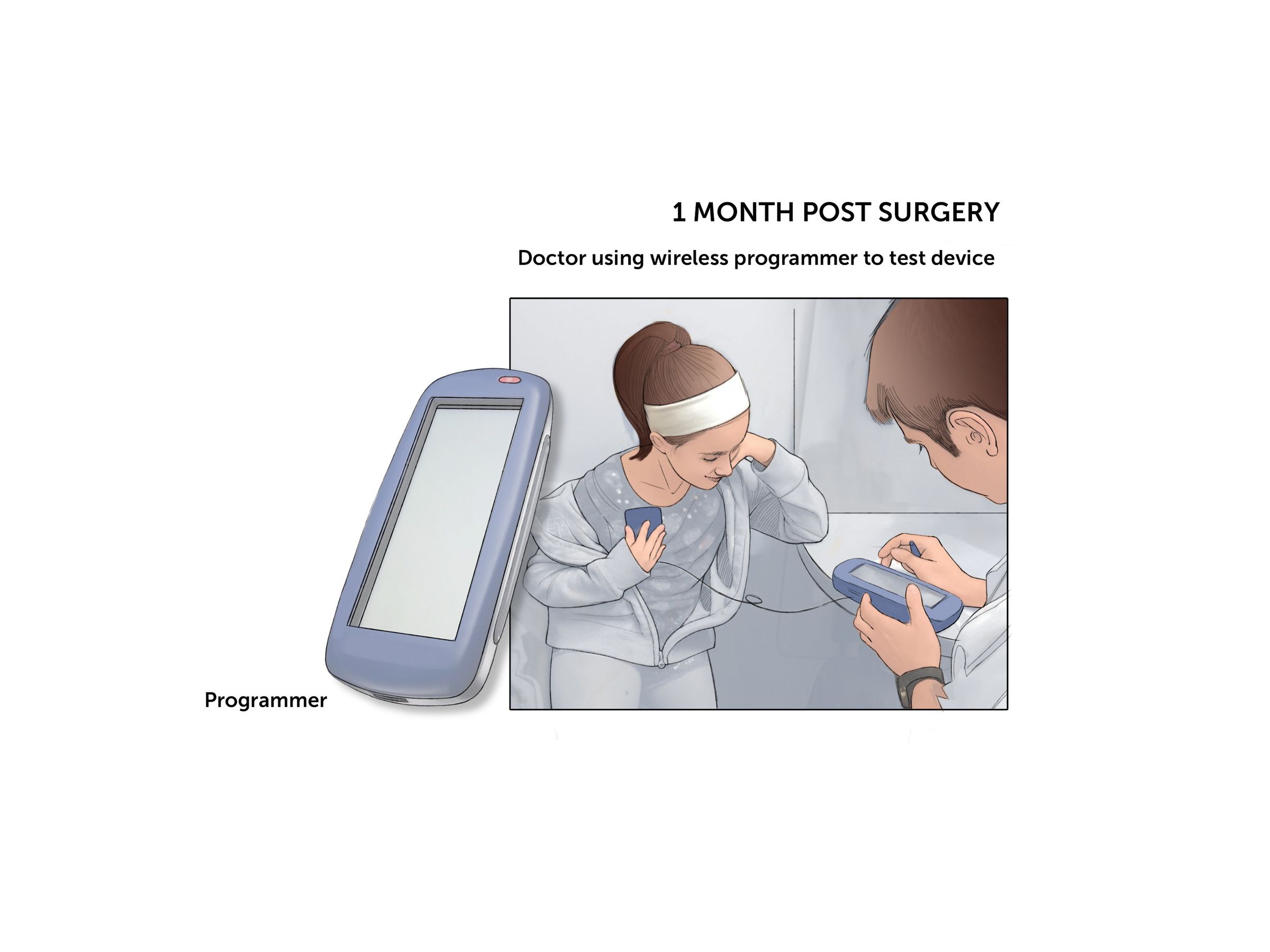
When the neurostimulator is turned on, it can give children with primary dystonia more control over their body movements. The settings are adjustable with a handheld wireless device, so the doctor can program the stimulator to the child’s individual needs. The family also receives a programming device to monitor and adjust the device as needed. The system can be safely removed at any time.
How DBS works isn’t completely known, but it has proven effective in several neurological disorders (not just dystonia). It is thought that the brain cells of children with primary dystonia signal too much, and that extra signals “spill over” to activate the wrong muscles. The electrical stimulation “dials back” these abnormal signals. DBS has been in use for more than 20 years, and according to the device manufacturer, more than 100,000 people around the world have received DBS therapy.
Because dystonia is relatively rare compared with disorders like Parkinson disease (the most common DBS application), the U.S. Food and Drug Administration (FDA) has granted approval under a Humanitarian Device Exemption. This designation is used for treatments that are recognized to be safe but that require further study in larger groups of patients to know how best to use them.
Frequently asked questions
Not all children with primary dystonia respond to DBS, but for those most suited to DBS, the therapy can reduce symptoms by 60 to 90 percent. Many children will have a noticeable, sometimes dramatic improvement in function, quality of life, and joint deformity. Occasionally, a child who has been wheelchair-bound may recover the ability to walk. Improvement isn’t immediate, though — it typically takes six to 12 months to see a substantial difference.
It’s important to note that DBS is not a cure, and abnormal movements will return when the system is turned off. This is true for all treatments for dystonia, not just DBS.
Under FDA criteria, DBS is indicated for children 7 or older. Children whose primary dystonia affects the whole body and is not controlled well by medications are the best candidates for DBS therapy. DBS can be used for generalized dystonia, hemidystonia (affecting one side of the body), segmental dystonia (affecting two adjacent parts of the body), and cervical dystonia (affecting the neck muscles).
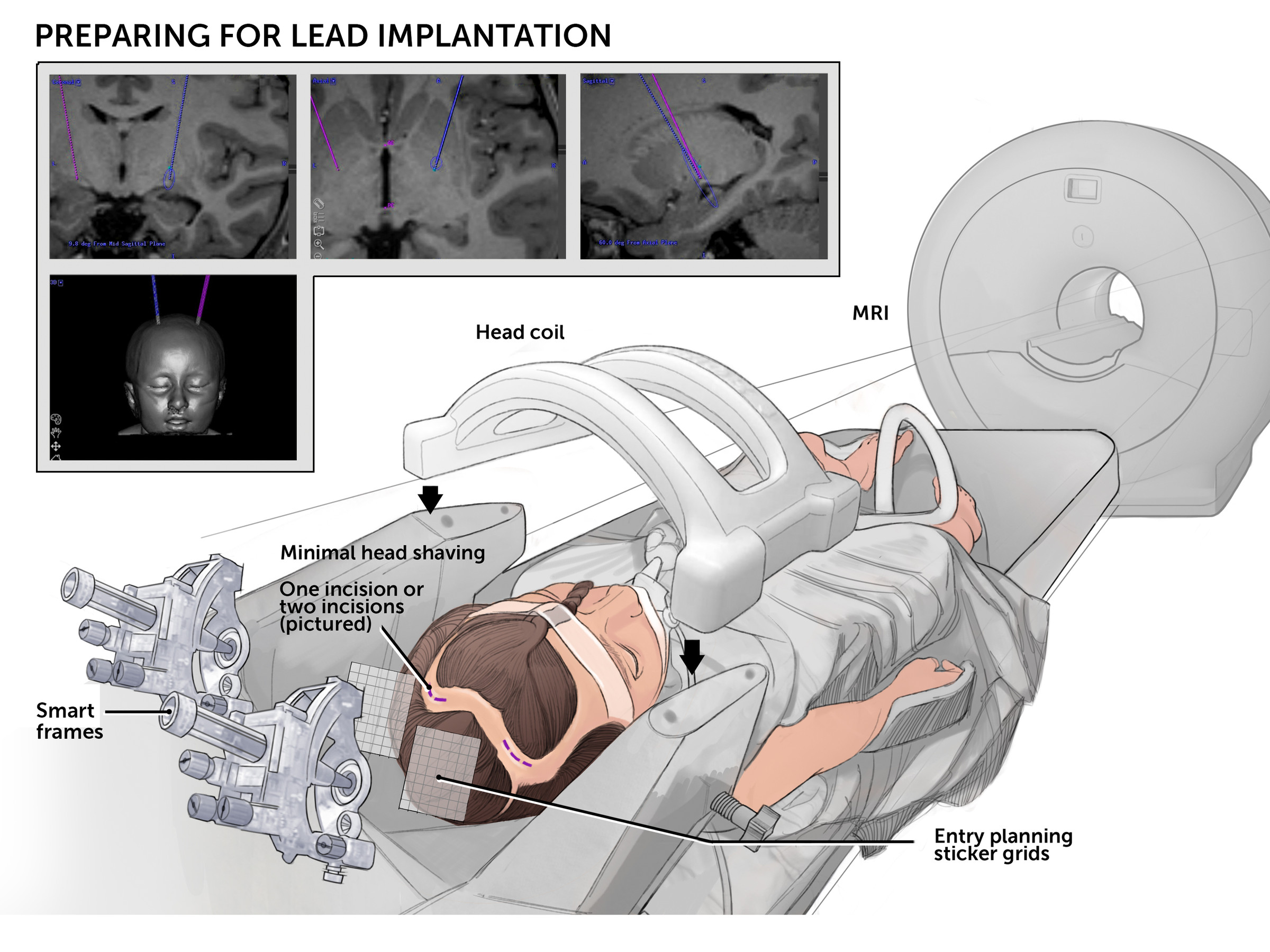
The children who do best with DBS tend to be younger and to start therapy before the symptoms cause permanent physical damage, such as joints that are fixed in place. At Boston Children’s, children with primary dystonia are carefully evaluated by movement disorder neurologist Jeff Waugh, MD, PhD, and neurosurgeon Scellig Stone, MD, PhD, to determine whether DBS might be of benefit. Each child is further evaluated with an MRI of the brain and neuropsychology testing. Our team then meets to confirm that surgery is appropriate and to discuss its optimal timing.
Currently available treatments for dystonia include physical therapy, oral medications, botulinum toxin (Botox) injections to affected muscles, and neurosurgery. These treatments alleviate symptoms, but none provide a cure. Botox works best for dystonia that affects a single area or only a few body parts but is insufficient for dystonias that are generalized throughout the body. There are other drugs with a body-wide effect, such as baclofen, a muscle relaxant, and trihexyphenidyl (Artane), which can relieve stiffness, tremors, and spasms. However, these drugs do not benefit all children and can have unwanted side effects.
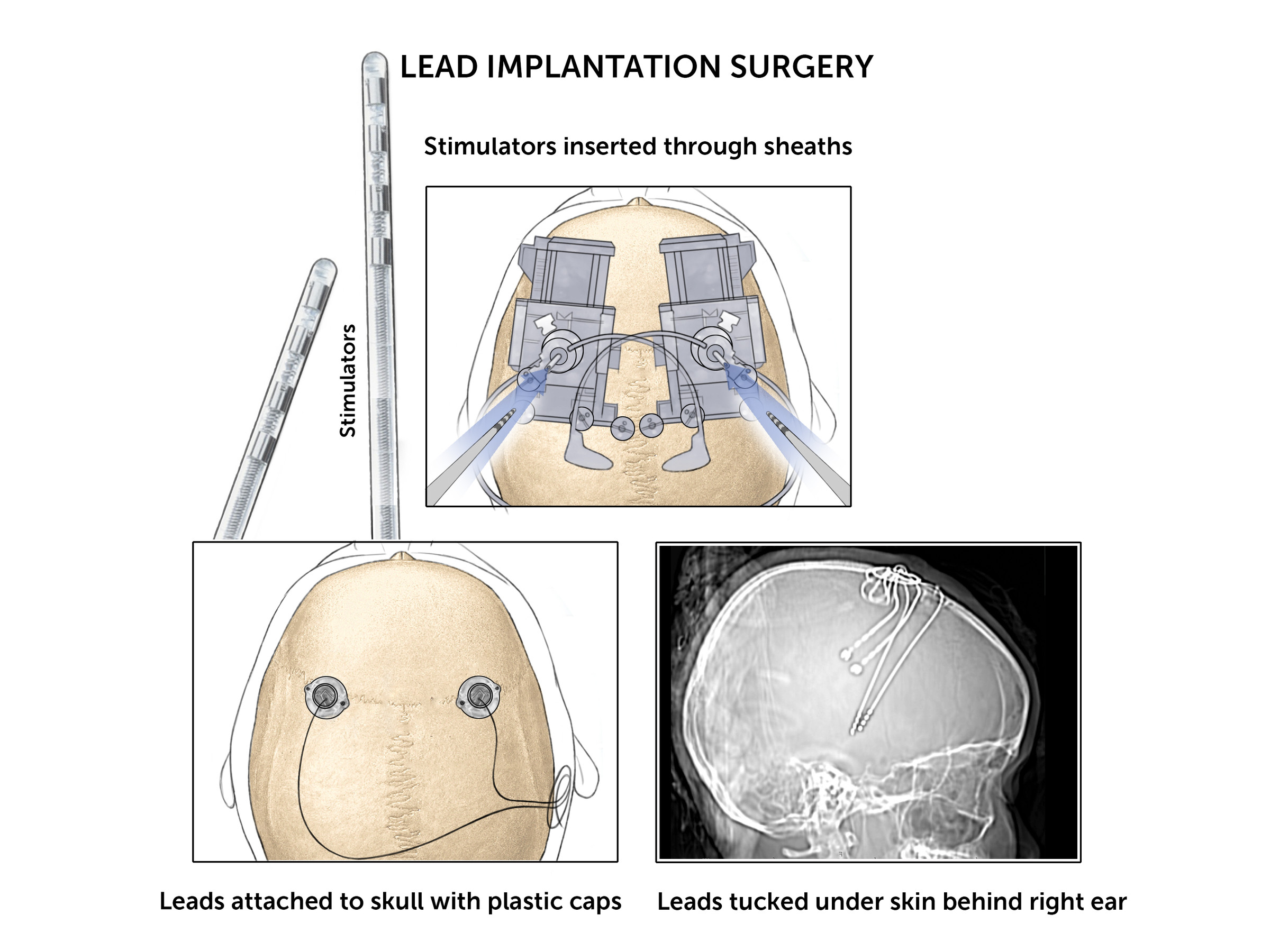
DBS therapy requires surgery to implant the neurostimulator, the leads, and the connecting wires (known as extensions). The surgery typically lasts several hours, while the child is asleep under general anesthesia, and requires a hospital stay.
The leads are inserted first, through a small opening in the skull, to a precisely targeted site within the brain. Usually, the extensions and neurostimulator are implanted and connected during the same procedure. (In rare cases, the extensions and the neurostimulator are implanted and connected in a separate operation.)
The neurostimulator usually isn’t turned on until the child has healed from the operation, typically four weeks after surgery. Once the device goes “live,” the settings will need to be tailored to each child. There is no “cookbook” for how DBS should be programmed, and every person’s ideal settings are different. This requires several follow-up visits — at first, every month after surgery, then every few months once the best settings have been determined.
The neurostimulator will need to be replaced every few years when its battery starts to run low. This is usually a minor outpatient operation. A rechargeable battery can be used in certain cases to lengthen battery life. The final DBS settings determine how much power output is needed and how long the battery will last.
Children with DBS systems need to follow some specific precautions; for example, they cannot have normal MRI scans, and there are situations in which the stimulator will need to be turned off. Your neurologist and neurosurgeon will review all these precautions with you.
As with any brain surgery and medical treatment, there are some risks to consider with DBS therapy. Your care team will discuss possible surgical complications and therapy side effects with you.
Research
Publications from Boston Children’s
- Stone SS; Alterman RL. Deep brain stimulation for dystonia. In: Youmans JR, Winn HR, editors. Youmans Neurological Surgery-7th edition. Philadelphia: Saunders/Elsevier; 2015. [in press]
- Waugh JL; Sharma N. Clinical neurogenetics: dystonia from phenotype to genotype (review). Neurol Clin 2013 Nov; 31:969-86. doi: 10.1016/j.ncl.2013.04.002.
- Waugh J; Sharma N. Pediatric movement disorders and ataxia. In: Sims K, Peters JM, Musolino P, Ward MZ, editors. Handbook of Pediatric Neurology. Philadelphia: Lippincott Williams & Wilkins; 2013.
- Stone SS; et al. Stimulation of entorhinal cortex promotes adult neurogenesis and facilitates spatial memory. J Neurosci 2011 Sep 21; 31:13469-84. doi: 10.1523/JNEUROSCI.3100-11.2011.