Congenital Fiber-Type Disproportion (CFTD) designates a heterogenous group of muscle disorders in which slow twitch (type 1) fibers are significantly (12 – 40%) smaller than their fast twitch (type 2) fiber counterparts (Clarke 2011; Kissiedu and Prayson 2016; Lawal, Todd, and Meilleur 2018). Affected individuals with CFTD tend to have scattered muscular weakness, low muscle tone, high arched palate, and bone deformities, as well as other medical issues that may include absent or low tendon reflexes and life-threatening respiratory problems (Clarke 2011; Clancy, Kelts, and Oehlert 1980; Kissiedu and Prayson 2016).
CFTD has been observed in congenital myopathies, as well as other disorders that affect the muscles (Clarke 2011; Clarke and North 2003). Since there are several conditions that can exhibit CFTD, it is often diagnosed after excluding other disorders (Kissiedu and Prayson 2016). CFTD is primarily diagnosed by taking a small muscle biopsy that is cut in very thin sections and stained with reagents that stain slow and fast twitch fibers differently. The stained muscle section is then observed under the microscope and an imbalance of fiber proportions would be suggestive of CFTD. In addition, fiber I predominance and absence of type IIB fibers have also been associated with CFTD (Clarke and North 2003).
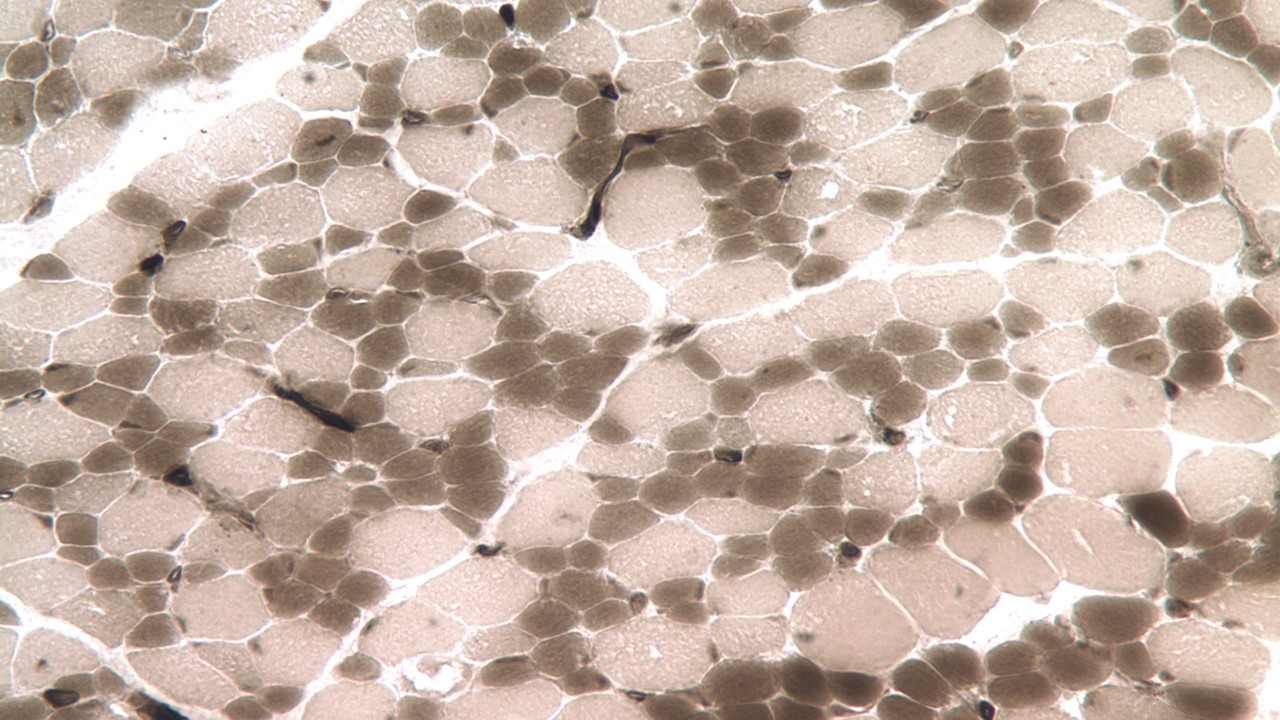
Slide of classic CFTD; with the darker type 1 fibers being much smaller than the lighter type 2 fibers.
Genetics
Cases of CFTD have been observed in several congenital myopathy subtypes, including those caused by mutations in the SELENON, TPM3, RYR1, ACTA1, TPM2, LMNA and MYH7 genes (Clarke 2011; Clarke et al. 2006; Clarke et al. 2010; Clarke et al. 2008; Kajino et al. 2014). The inheritance pattern of CFTD depends on the affected gene. For instance, CFTD may be inherited in a dominant pattern if the affected gene is ACTA1, whereas it may be inherited in an autosomal recessive pattern if the affected gene is either SELENON or RYR1 (Lawal, Todd, and Meilleur 2018; Clarke and North 2003). On the other hand, mutations in the TPM3 may result in an inheritance pattern of either recessive or dominant (Lawlor et al. 2010). Very rarely has CFTD been observed to be inherited in an X-linked pattern (Clarke et al. 2005).
Research
One of the goals of the research done at the Beggs laboratory is to identify the genes causing CFTD. The study of the proteins coded by those genes will allow us to unravel the pathophysiology of this group of disease which will be crucial for improving diagnosis and treatment of this condition in the future. If you are the parent of a child with a congenital myopathy, if you yourself are affected, or if you are the healthcare provider of someone with CFTD, you may be able to help us better understand CFTD and to determine the genetic changes associated with the condition.
References
Clancy, R.R., K. A. Kelts, and J. W. Oehlert. "Clinical Variability in Congenital Fiber Type Disproportion." J Neurol Sci 46, no. 3 (1980): 257-66.
Clarke, N. F., R. L. Smith, M. Bahlo, and K. N. North. "A Novel X-Linked Form of Congenital Fiber-Type Disproportion." Ann Neurol 58, no. 5 (2005): 767-72.
Clarke, N. F. "Congenital Fiber-Type Disproportion." Seminars in Pediatric Neurology 18, no. 4 (2011): 264-71.
Clarke, N. F., W. Kidson, S. Quijano-Roy, B. Estournet, A. Ferreiro, P. Guicheney, J. I. Manson, A. J. Kornberg, L. K. Shield, and K. N. North. "Sepn1: Associated with Congenital Fiber-Type Disproportion and Insulin Resistance." Annals of Neurology 59, no. 3 (2006): 546-52.
Clarke, N. F., H. Kolski, D. E. Dye, E Lim, R. L. L. Smith, R. Patel, M. C. Fahey, R. Bellance, N. B. Romero, E. S. Johnson, A. Labarre-Vila, N. Monnier, N. G. Laing, and K. N. North. "Mutations in Tpm3 Are a Common Cause of Congenital Fiber Type Disproportion." Annals of Neurology 63, no. 3 (2008): 329-37.
Clarke, N. F. and K. N. North. "Congenital Fiber Type Disproportion—30 Years On." Journal of Neuropathology & Experimental Neurology 62, no. 10 (2003): 977-89.
Clarke, N. F., L. B. Waddell, S. T. Cooper, M. Perry, R. L. L. Smith, A. J. Kornberg, F. Muntoni, S. Lillis, V. Straub, K. Bushby, M. Guglieri, M. D. King, M. A. Farrell, I. Marty, J. Lunardi, N. Monnier, and K. N. North. "Recessive Mutations in Ryr1 Are a Common Cause of Congenital Fiber Type Disproportion." Human mutation 31, no. 7 (2010): E1544-E50.
Kajino, S., K. Ishihara, K. Goto, K. Ishigaki, S. Noguchi, I. Nonaka, M. Osawa, I. Nishino, and Y. K. Hayashi. "Congenital Fiber Type Disproportion Myopathy Caused by Lmna Mutations." J Neurol Sci 340, no. 1-2 (2014): 94-8.
Kissiedu, J. and R. A. Prayson. "Congenital Fiber Type Disproportion." J Clin Neurosci 26 (2016): 136-7.
Lawal, T. A., J. J. Todd, and K. G. Meilleur. "Ryanodine Receptor 1-Related Myopathies: Diagnostic and Therapeutic Approaches." Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics 15, no. 4 (2018): 885-99.
Lawlor, M. W., E. T. Dechene, E. Roumm, A. S. Geggel, B. Moghadaszadeh, and A. H. Beggs. "Mutations of Tropomyosin 3 (Tpm3) Are Common and Associated with Type 1 Myofiber Hypotrophy in Congenital Fiber Type Disproportion." Human mutation 31, no. 2 (2010): 176-83.
This page was last updated October 23, 2020.