Non-Specific Congenital Myopathies | Overview
The congenital myopathies are rare disorders that result in muscle weakness of variable severity (North et al. 2014). Some patients are affected from birth, while others may develop symptoms in childhood or adulthood (Colombo et al. 2015). Although patients with some types may not survive past the first few years of life, others may walk independently through adulthood and have families of their own (North et al. 2014).
The diagnosis of congenital myopathies is usually made from a muscle biopsy (Ravenscroft, Laing, and Bonnemann 2015). Sometimes, specific muscle changes such as rods or tubules are found in these biopsies; however, around one-third of the biopsies taken do not reveal any specific changes and therefore no specific diagnosis can be established in those cases (Ravenscroft et al. 2018; Bohm et al. 2013). Our laboratory is interested in studying DNA and muscle biopsy samples of these patients since it would provide insight into the genetic causes of their muscular conditions.
Identification of these genes could have direct clinical benefit to patients and their families by allowing specific diagnostic testing such as carrier detection and prenatal diagnosis for those who wish. Furthermore, understanding the genetic cause(s) of congenital myopathies will increase our understanding of muscle biology and provide insights into future development of specific treatments and therapies.
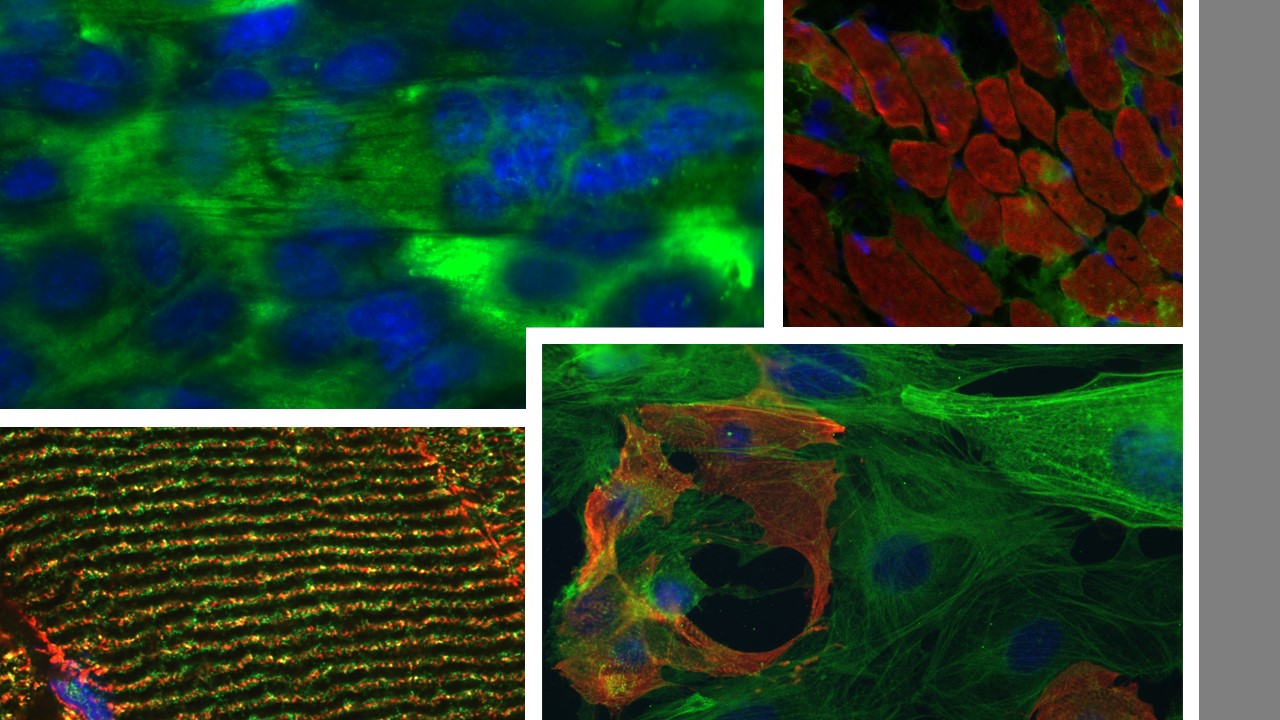
Using various fluorescent stains to help diagnosis non-specific congenital myopathies.
Genetics
Most congenital myopathies are thought to have a genetic cause (Colombo et al. 2015; North et al. 2014; Ravenscroft et al. 2018). This means that the condition is caused by alterations in certain genes that are involved in muscle function and/or development. Despite the genetic cause of these diseases, most often, congenital myopathies happen in families where no previous history of neuromuscular disorders has been reported. In these cases, we say that the genetic condition occurred sporadically. Although genetic changes can arise sporadically, once the change appears in a person's genes, the alteration can be passed on from an affected parent to children in a specific pattern of inheritance (Bohm et al. 2013). Inheritance patterns may vary among different families. It is the purpose of our study to understand these alterations, how they can arise and how they are inherited.
Research
One of the goals of the research done at the Beggs laboratory is to identify genes causing congenital myopathies with non-specific muscle changes. We hope that what we learn will be useful for improving diagnosis and treatment of these conditions. If you are the parent of a child with a congenital myopathy, if you yourself are affected, or if you are the healthcare provider of a patient with this condition, you may be able to help us to better understand these neuromuscular conditions, and to develop better tests, therapies and treatments.
References
Bohm, J., N. Vasli, E. Malfatti, S. Le Gras, C. Feger, B. Jost, N. Monnier, J. Brocard, H. Karasoy, M. Gerard, M. C. Walter, P. Reilich, V. Biancalana, C. Kretz, N. Messaddeq, I. Marty, J. Lunardi, N. B. Romero, and J. Laporte. 2013. 'An integrated diagnosis strategy for congenital myopathies', PLOS ONE 8: e67527.
Colombo, I., M. Scoto, A. Y. Manzur, S. A. Robb, L. Maggi, V. Gowda, T. Cullup, M. Yau, R. Phadke, C. Sewry, H. Jungbluth, and F. Muntoni. 2015. 'Congenital myopathies: Natural history of a large pediatric cohort', Neurology 84: 28-35.
North, K. N., C. H. Wang, N. Clarke, H. Jungbluth, M. Vainzof, J. J. Dowling, K. Amburgey, S. Quijano-Roy, A. H. Beggs, C. Sewry, N. G. Laing, and C. G. Bonnemann. 2014. 'Approach to the diagnosis of congenital myopathies', Neuromuscul Disord 24: 97-116.
Ravenscroft, G., R. J. Bryson-Richardson, K. J. Nowak, and N. G. Laing. 2018. 'Recent advances in understanding congenital myopathies', F1000Res, 7.
Ravenscroft, G., N. G. Laing, and C. G. Bonnemann. 2015. 'Pathophysiological concepts in the congenital myopathies: blurring the boundaries, sharpening the focus', Brain 138: 246-68.
This page was last updated October 23, 2020.
