Department of Surgery | Pediatric Surgery Fellowship
Boston Children’s Hospital has a long and rich tradition of training the leaders in pediatric surgery. Our fellowship is the first training program, offered by the largest department of pediatric surgery in the country. We combine this history with a dedication to pushing the field forward as a leader in education, innovation, research, and clinical care.
The fellowship is a two-year clinical training program for which we have three ACGME-approved positions.
One resident is selected to begin training on odd years, and two residents are selected to begin training on even years. Residents are selected through the Electronic Residency Application Service (ERAS). Applicants must have completed a general surgical training program by time of matriculation and must be eligible to take the qualifying examination in general surgery given by the American Board of Surgery or the Royal College of Surgeons of Canada.
Fellows are involved in a high volume of straightforward procedures, many of which employ minimally invasive techniques. Because we are a referral center, our fellows also gain hands-on experience treating complex cases. Operative experience includes thoracic, abdominal, urologic, oncologic, vascular, endoscopic, and transplant surgery. The fellows clinic (Index Clinic) offers residents the opportunity to regularly participate in outpatient evaluation and postoperative follow-up of pediatric surgical diseases.
The program is structured to offer residents a total of 16 months of their 24-month tenure as the chief on one of our two services, working closely with senior staff and their co-fellows in all aspects of patient management on the surgical floors, ICU, and NICU. A staff of more than a dozen pediatric nurse practitioners provide the chief residents with experienced and reliable care of their inpatients. In addition, one of the chief residents functions as the administrative chief resident, helping to organize the operating room schedule, a large surgical resident and medical student contingent, and a robust educational conference schedule. Administrative staff in the department help the chief residents with these tasks.
Teams
The Pediatric General Surgery Service is divided into two separate teams, the Gross and Ladd services, in order to group patients according to their primary disease process (e.g. short bowel syndrome, transplant, esophageal atresia). There is a chief pediatric surgery fellow assigned to each service.
The two-service-team approach allows us to more evenly distribute the number of inpatients that are cared for by the fellows, residents, interns, and nurse practitioners.
The team includes:
- general surgery senior residents (2-4 residents a month) who rotate from area hospitals, including Brigham and Women’s Hospital, Beth Israel Deaconess Medical Center, Boston Medical Center, Lahey Hospital & Medical Center, St. Elizabeth Medical Center, and Tufts Medical Center
- two to three general surgery interns
- a large group of more than a dozen nurse practitioners who cover the service 24/7
- one to three critical care surgical fellows assigned to the NICU/MSICU
- eight to 10 surgical research fellows who assist with call coverage at night
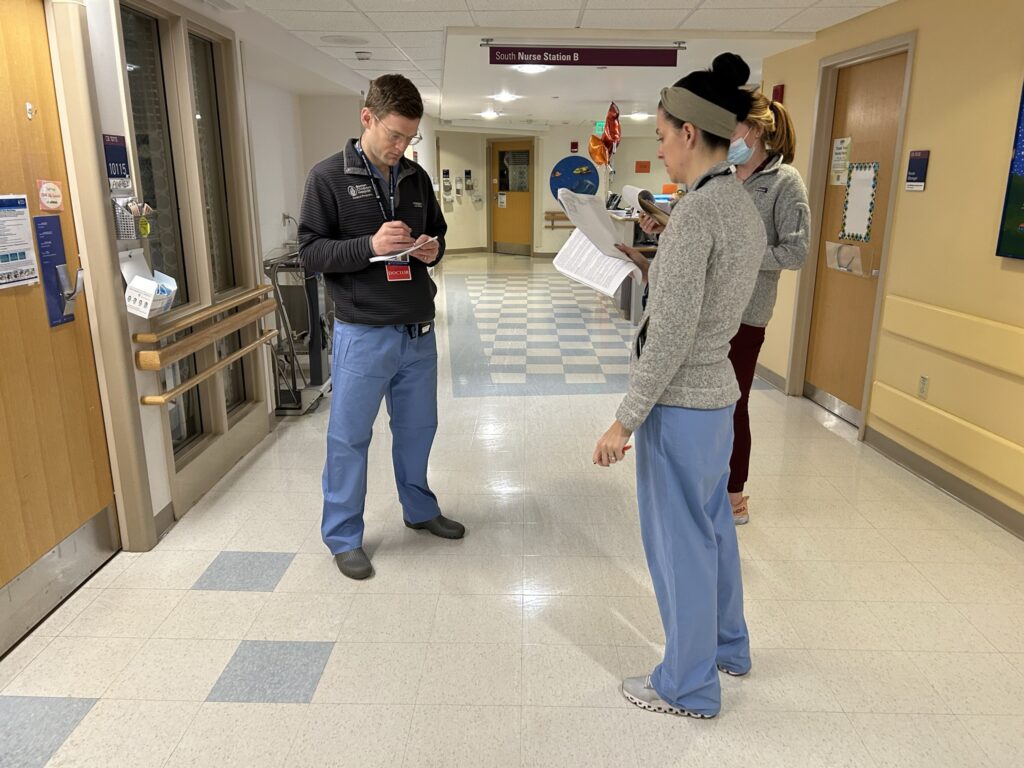
Pediatric Surgery Fellowship Rounds
Morning rounds
Each team is composed of one fellow, one senior resident, one intern, and two nurse practitioners, and either the surgeon of the week (SOW) or senior fellow (+/- additional senior/intern residents).
- 5:45 a.m.: overnight sign out
- 6 a.m.: floor rounds begin
- 6:45 a.m.: ICU rounds begin
- 7:15 a.m.: chiefs, SOW, and surgeon of the day (SOD) meet for sign out
- 5:30 p.m.: evening sign-out
Overnight call
- A fellow is on call in the hospital one to two times per week acting as a pre-attending.
- Fellows are on call from home available for urgent inpatient concerns or fellow level OR cases at their discretion.
