Ongoing Research | Overview
Our laboratory studies the pathophysiology of organ injury driven by myeloid cells in sepsis and surgical induced systemic inflammation. In addition, we have been studying the role of anesthetics in perioperative immune function and their outcomes.
Anesthetics-mediated immunomodulation
We are interested in understanding perioperative immune function because its adequacy is critical for proper host defense. We primarily focus on the impact of anesthetic choice on the occurrence of surgical site infections. Anesthetics, particularly volatile anesthetics are often provided to patients. Although the anesthetic mechanism of volatile anesthetics remains to be determined, these promiscuous molecules are suggested to affect the function of immune cells. We reported that they directly interacted with and inhibited adhesion molecule family integrins (Figure 1).

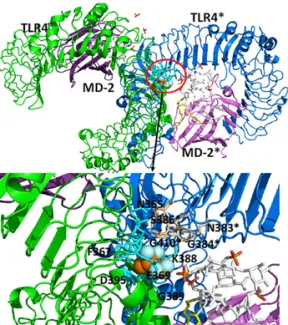
In addition, we found that they directly bound to critical pattern recognition receptors Toll-like receptors 2 and 4 (TLR2/TLR4) (Figure 2). We have shown in vivo that prolonged volatile anesthetic exposure was associated with higher bacterial loads. Our ultimate goal is to understand the impact of anesthetics and propose anesthetic regimens based on patients’ underlying diseases.
Sepsis and integrins
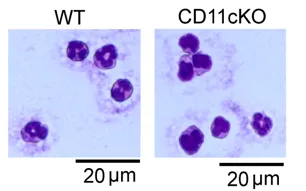
Sepsis remains to be a disease with high morbidities and mortalities. Although neutrophils are the first line innate immune cells to eradicate infection as host defense mechanism, we have increasingly recognized that neutrophils are heterogeneous population. We are currently investigating the novel role of β2 integrins αXβ2 and αDβ2 in neutrophil pathophysiology. Our study showed that αXβ2 regulates neutrophil maturation (Figure 3).