Neuromuscular Scoliosis | Symptoms & Causes
What are the symptoms of neuromuscular scoliosis?
Signs of neuromuscular scoliosis often appear early in a child’s life. You, your child’s doctor, or another caregiver will most likely notice your child’s spinal curve through a change in their overall body position or when they start having trouble sitting in a chair. Symptoms may include:
- leaning or uneven seating posture
- using arms for seating support
- uneven shoulder heights
- head off center from the rest of the body
- uneven hips or buttocks
- uneven shoulder blades
- arms hanging unevenly

Meet Colin
Born with a rare neuromuscular disorder, he spent his first months in the ICU struggling to breathe. Spinal surgery for neuromuscular scoliosis and a drive to keep up with his sisters helped him to swim, ski, and play.
Neuromuscular Scoliosis | Diagnosis & Treatments
How is neuromuscular scoliosis diagnosed?
Your child’s doctor will use medical and family histories, physical exams, and diagnostic tests to determine the nature, extent, and impact of your child’s scoliosis. They will also evaluate your child’s underlying neuromuscular disease, including their:
- nutritional status
- lung and heart function
- functional level
- joints and extremities (for contractures)
- balance and ability to walk (also known as ambulatory level)
Doctors can often predict the likely progression of a child’s scoliosis. They do this by assessing the severity of the existing curve and comparing that to the child’s stage of growth. Mild or moderate curves can become more pronounced during growth spurts. Children at a later stage of growth may be less prone to further spinal deformity.
Diagnostic tests
X-ray images taken from the front and side are the main tool for confirming neuromuscular scoliosis and the severity of the curve.
Your child’s doctor may also order one or more of the following tests to evaluate the underlying condition associated with the scoliosis:
- magnetic resonance imaging (MRI)
- computerized tomography scan (CT or CAT scan)
- EOS imaging
- blood tests
- ultrasound
- bone scans
- bone density scans (dual-energy x-ray absorptiometry, DEXA, DXA)
- muscle biopsy
- pulmonary function tests
- electromyogram (EMG) and nerve conduction studies
What are the treatment options for neuromuscular scoliosis?
Non-surgical treatments
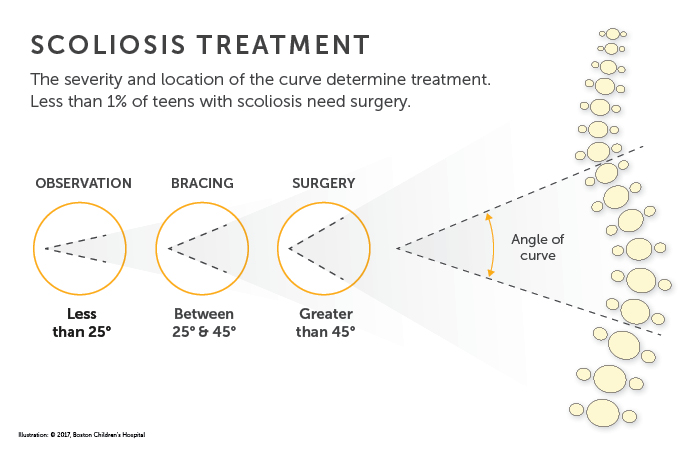
Non-surgical treatments such as bracing, wheelchair modification, physical therapy, and environmental adaptation can help your child adapt to everyday environments and improve their mobility. Bracing can prevent your child’s spinal curvature from getting worse during periods of growth, but bracing will not correct the curve.
Spinal fusion surgery
Stabilizing the spine with spinal fusion surgery is the most common treatment for neuromuscular scoliosis. Using metal rods, hooks, screws, and wires, known as instrumentation, the procedure straightens the spine and solidifies the bone so it will no longer curve abnormally. For six to 12 months after surgery, the spine fuses in much the same way that a broken bone heals. The child will need to wear a brace during this time. The instrumentation typically remains in the back without causing any problems.
The goal of a spinal fusion surgery for neuromuscular scoliosis is to:
- stabilize the curve and stop its progression
- balance the spine and pelvis (in patients who are unable to walk)
- restore the ability to sit upright (in children who have lost this ability)
- improve/preserve lung function
Spinal fusion for neuromuscular scoliosis is usually necessary by the time a child reaches adolescence — often sooner than with idiopathic scoliosis. Compared to idiopathic scoliosis, it is usually necessary to fuse a larger portion of the spine in order to correct neuromuscular scoliosis.
Because children with neuromuscular scoliosis have a higher rate of complications, quality and safety are critical at each stage of the surgery — from preoperative planning all the way through recovery. Research has shown that the involvement of a multidisciplinary team of specialists can reduce the risk of complications.
What is the long-term outlook for children with neuromuscular scoliosis?
A child’s outlook depends less on their scoliosis and more on the nature, severity, and overall impact of their neuromuscular disease. With successful surgery and attentive post-operative care, your child can:
- return to the functional level they had reached before they needed surgery
- have a straighter, more balanced spine
- find it easier to sit up
- have the potential for improved lung function and decreased susceptibility to pneumonia
How we care for neuromuscular scoliosis
The Spine Division at Boston Children’s Hospital is the largest and busiest pediatric spine center in the United States. With a focus on quality and safety, our spine specialists see thousands of spine patients and perform hundreds of spine surgeries each year. We treat all types of scoliosis and other spine conditions, from the most common to the most complex.
We also work closely with Boston Children’s Department of Neurology and the Care for Children with Medical Complexity program to correct complex spine deformities that involve the spinal cord. This multidisciplinary approach to care helps ensure that every patient receives the highest quality care, no matter how complex their surgical, medical, and behavioral needs.

