Lordosis | Symptoms & Causes
What are the symptoms of lordosis?
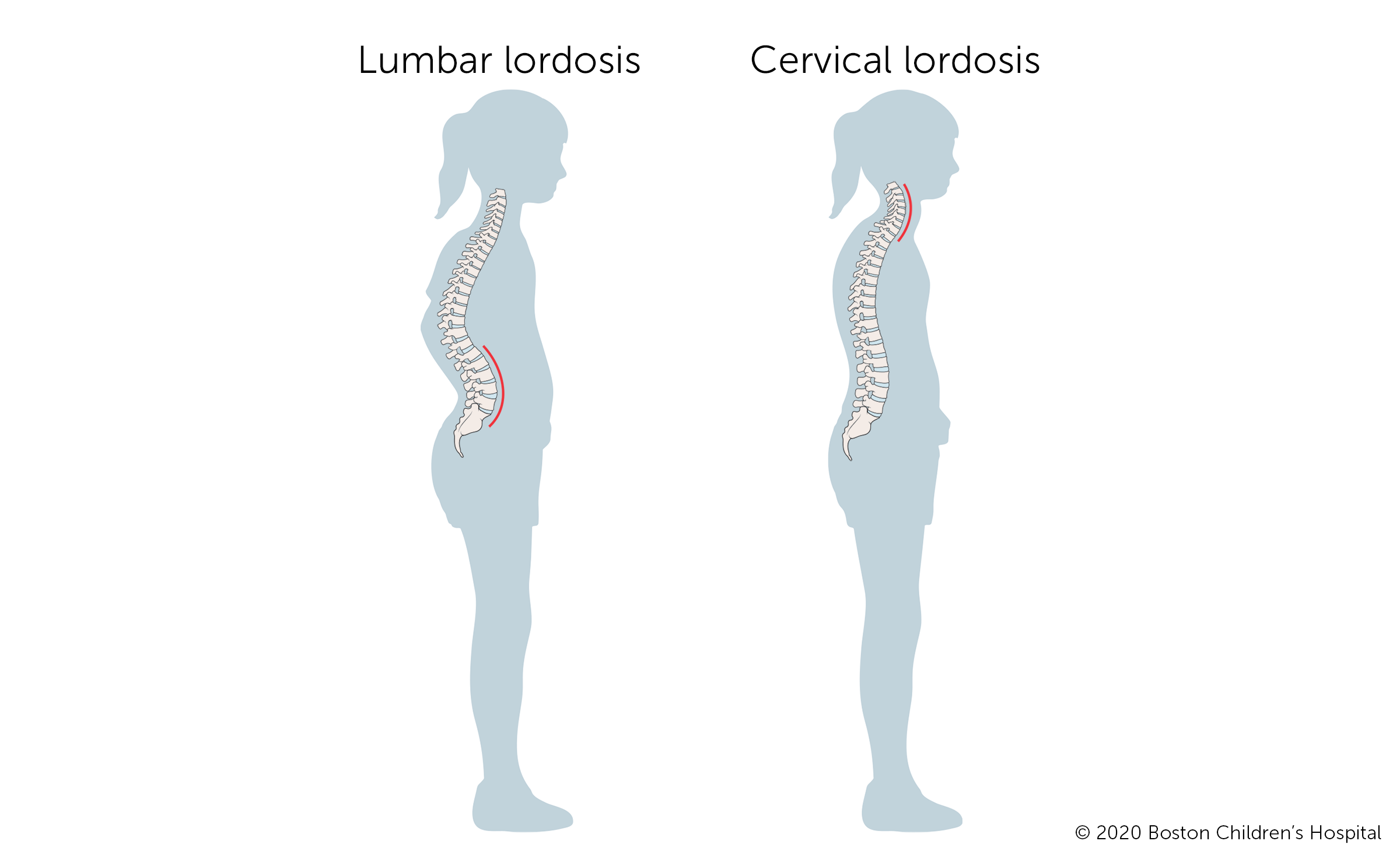
Children with lordosis have a swayback appearance. Their posture may seem exaggerated. Their buttocks may sway further out to the back than normal and their stomachs sway out in front. When a child with lumbar lordosis lays on their back, it may be difficult or impossible for them to press their lower back into the floor.
In rare cases, children with severe lordosis may have pain, numbness, tingling, or weakness in one or both of their legs. They may also lose control of their bladder. If your child has these symptoms, they should be seen by a spine specialist as soon as possible.
What causes lordosis?
In many cases, doctors don’t know the cause of lordosis. While lordosis tends to develop during adolescence, some children are born with a higher risk of developing the condition. Lordosis is often associated with one of the following:
- Posture: The lumbar spine relies on the muscles around the stomach and lower back (abdominal muscles) for support. Children with weak abdominal muscles tend to be more prone to lordosis.
- Overweight: Extra weight in the belly puts strain on the lower back and pulls it forward, increasing the risk for lordosis.
- Trauma: Sports injuries, accidents, or serious falls can cause spondylolysis, a type of spinal fracture. This can weaken the spine and cause the affected vertebrae to curve at a more extreme angle.
- Surgery: Selective dorsal rhizotomy, a minimally invasive surgery that may be used to reduce leg spasticity in some patients with cerebral palsy, can lead to lordosis.
- Neuromuscular conditions: Children with conditions that impair nerve and muscle function may also develop lordosis. Such conditions include muscular dystrophy, cerebral palsy, and several others.
- Hip problems: Some children with hip dysplasia also develop lordosis.
Lordosis | Diagnosis & Treatments
How is lordosis diagnosed?
Your child’s doctor will conduct a full medical history, physical exam, and diagnostic tests to confirm lordosis. The medical history will include questions about any other close family members diagnosed with lordosis or other spine problems.
Diagnostic tests may include:
- X-ray, a diagnostic test that uses electromagnetic energy beams to produce images of internal tissues, bones, and organs. Your child’s doctor will use the x-ray to determine the degree of your child’s spinal curvature.
- CT or CAT scan (computerized tomography scan), a diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images of the body. CT scans show detailed images of any part of the body, including the bones, muscles, fat, and organs and are more detailed than general x-rays.
- MRI (magnetic resonance imaging), a diagnostic procedure that uses a combination of large magnets, radio frequencies, and a computer to produce detailed images of organs and structures within the body.
- Bone scan, an imaging method used to determine the cause of bone pain or inflammation, evaluate changes in the joints, and detect bone diseases and tumors.
- Blood tests are sometimes used to look for associated metabolic conditions. They are not a standard part of diagnosing lordosis, however.
How is lordosis treated?
In most cases, lordosis is not painful and does not cause mobility problems. Close monitoring, preferably by a spine specialist, will help detect and manage any progression of the curve. This is particularly important during growth spurts.
If your child’s lordosis is related to a condition such as spondylolysis, muscular dystrophy, or achondroplasia, their treatment may focus on the primary condition while also managing the symptoms of lordosis.
Depending on your child’s age, stage of growth, and the degree of their curve, their doctor may prescribe one or more of additional treatments.
- Physical therapy, which uses exercise to reduce pain, improve physical function, and develop the muscles in the back so they can better support the spine.
- Bracing, which can stabilize the back and prevent the spine from becoming more curved. Your child’s doctor may recommend bracing if their curve is growing or is greater than 30 degrees.
- Spine surgery is only necessary for severe cases of lordosis.
What is the long-term outlook for children with lordosis?
With early detection, proper monitoring, and appropriate treatment, most children and adults with lordosis live full, active lives.
How we care for lordosis at Boston Children’s Hospital
The Spine Division at Boston Children’s Hospital is the largest and busiest pediatric spine center in the United States. Each year, we treat thousands of patients with spine conditions that range from simple to complex. Whenever possible, we provide non-surgical treatment for lordosis. In the rare cases that require surgery, we are a center of excellence in surgical procedures of the spine. When appropriate, our Spine and Sports Program works with young athletes with lordosis that is the result of a sports injury, with a focus on recovery and safe return to play.