Inflammatory Bowel Disease | Symptoms & Causes
What are the symptoms of inflammatory bowel disease?
The symptoms of inflammatory bowel disease (IBD) depend on the individual child but may include:
- diarrhea, especially if bloody
- obvious blood in the stools or black, tar-like stools
- abdominal pain
- fatigue
- weakness
- weight loss
- loss of appetite
- rectal bleeding
- loss of body fluids and nutrients
- anemia caused by severe bleeding
- unexplained fevers
- vomiting
Sometimes children also experience:
- joint pain
- inflammation of the eyes
- liver disorders
- osteoporosis
- rashes
- kidney stones
- mouth ulcers
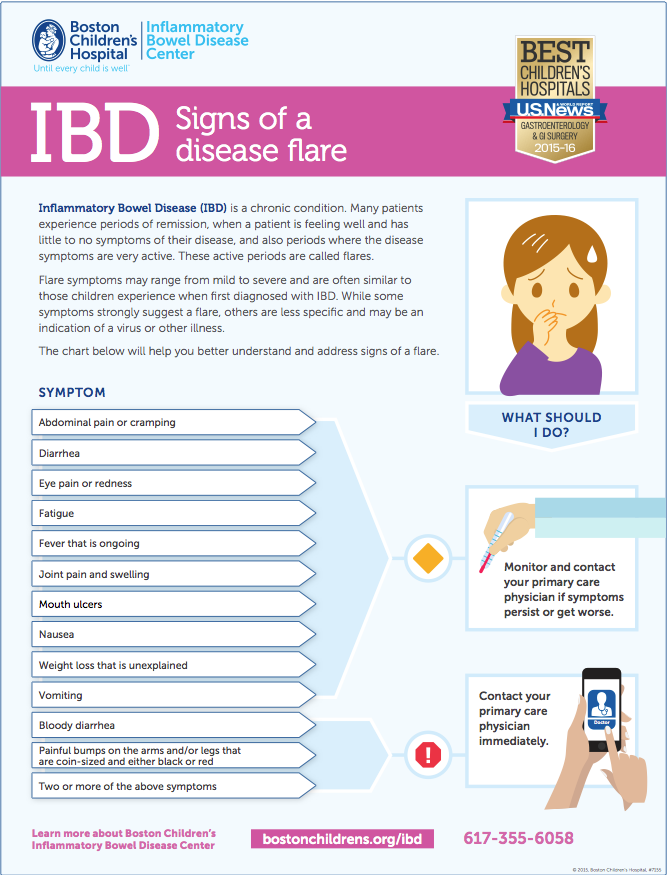
IBD typically includes periods of remission (when no symptoms occur) and flare-ups (recurrence of one or more of the symptoms that originally led your child to be diagnosed with IBD, such as diarrhea, rectal bleeding, and cramping). Most people with IBD experience occasional flares.
What causes inflammatory bowel disease?
The causes of IBD are still unclear but likely include a combination of genetic and environmental factors with immune system dysfunction.
Inflammatory Bowel Disease | Diagnosis & Treatments
How is inflammatory bowel disease diagnosed?
The first step in treating inflammatory bowel disease (IBD) is to figure out whether or not your child has Crohn’s disease, ulcerative colitis, or another type of IBD. To do that, a doctor will take a careful medical history and perform a physical exam. Some other tests might also be needed, such as:
- Blood tests. Providers may test your child’s blood to help diagnose IBD and to see how well treatment is working. Tests include those that measure hematocrit (the ratio of red blood cells to total blood cells), white blood cells, platelets, and C-reaction protein (a measure of inflammation).
- Stool sample. Your child’s doctor may ask you to provide a sample of their bowel movements to look for inflammation or infections.
- Endoscopy. An upper endoscopy looks inside the esophagus (food pipe), stomach, and the beginning of the small intestine. The doctor will pass a long, flexible tube with a light on the end through the mouth and esophagus and into the stomach and small intestine. As the doctor passes the tube, they look at these areas and may take small samples of tissues, which are called biopsies.
- Colonoscopy. This test also uses a thin, flexible tube with a light and camera lens at the end to examine the inside of the large intestine. As the doctor passes the tube through the rectum, they look at the areas of the intestine and also may take biopsies.
- Imaging studies. CT scans and MRI scans
What are the treatment options for inflammatory bowel disease?
While IBD is a lifelong condition, the goal is to keep it in remission for as long as possible so that your child experiences few to no symptoms. Your child’s care team may use a variety of treatment and maintenance approaches, such as:
Dietary changes
Dietary interventions are currently being studied to assess the best diet for improving inflammation. Avoiding certain foods, or following certain diets, in conjunction with medication, can help control symptoms. A dietician can design a balanced nutrition program for your child.
Medications
Your child’s doctor will likely prescribe one or more maintenance medications to treat IBD and prevent flares. There are three main classes of maintenance medications for IBD:
Aminosalicylates (5-ASAs): These are aspirin-like medications that decrease inflammation at the intestine wall itself. They are most often used in mild-to-moderate ulcerative colitis and occasionally in Crohn’s disease. Examples of 5-ASAs include mesalamine (Asacol, Rowasa, Pentasa, Colazal, Lialda, Apriso, and Delzicol), sulfasalazine, and balsalazide.
Immunomodulators: This is a type of medication used to treat Crohn’s disease and ulcerative colitis by decreasing immune system activity. The most commonly used immunomodulators are 6-mercaptopurine (6MP), azathioprine (Imuran), and methotrexate. Less commonly used immunomodulators include tacrolimus (Prograf) and cyclosporine (Noral, Sandimmune). These agents are typically used in patients who do not respond to other treatments. Your child’s doctor will check his or her lab work closely when starting these medications.
Biologics: These medications are used when IBD does not respond to other medications, when other medications cause side effects, or if your child has complications of Crohn’s or ulcerative colitis, such as refractory disease or fistulas. Biologics work by blocking inflammatory chemicals in the blood. They may also decrease the number of immune system cells in the body. Examples of this class of medications include Remicade, Humira, Cimzia, Simponi, Sterlara, and Entyvio. These medications are usually given as injections or infusions.
Your child’s doctor may also prescribe steroids. These medications are used to reduce inflammation during a flare and to relieve diarrhea, rectal bleeding, fever, and pain in both forms of IBD. They can also relieve systemic symptoms like joint pain and skin and eye lesions in some patients. Typically, these are used during a flare to quiet symptoms while finding the correct maintenance medication for your child. There are different types of steroids, including:
- intravenous steroids, which are given in the hospital
- oral steroids, such as prednisone, which tend to have more systemic effects
- topical steroids, which treat localized inflammation in the sigmoid colon, rectum, or anus by using an enema, foam, or suppository; these tend to have fewer side effects than oral/IV steroids
Antibiotics are sometimes used to treat infections, fistulas, and abscesses. They can also be used in conjunction with other medications for Crohn’s disease. The most commonly used antibiotics include metronidazole and ciprofloxacin.
Surgery
While doctors almost always start treatment for IBD with medication, sometimes a child may not respond — or may stop responding — to medications and be a good candidate for surgery. The decision to have surgery is a joint one, made between your child, your family, your child's gastroenterologist, and the surgeon.
In Crohn’s disease, a surgical procedure called a resection, which removes a section of the intestine, may be considered. However, it's important to remember that with Crohn's disease, surgery is rarely a cure, since inflammation may recur in other locations throughout the digestive tract. The purpose of surgery is to keep your child feeling well, to minimize the damage done to the intestine, or to remove a piece of the intestine that is extremely damaged so that medications can work more effectively.
A small percentage of children with ulcerative colitis who do not respond to medication may need surgery, which can dramatically improve quality of life and improve symptoms. This surgery, called a colectomy, removes some or all of the large intestine and modifies the small intestine to create a new rectum.
What are the treatment options for VEO-IBD?
Children with VEO-IBD typically don’t respond well to standard therapy for IBD. For this reason, researchers are actively studying treatment options for these children. The following approaches have proven effective for some children with VEO-IBD:
Medication: Children with VEO-IBD who have a mutation in the NCF2 gene respond well to antibiotics. Those with mutations in the LRBA gene experience improved symptoms after using abatacept, a medication that interferes with T cells and is more commonly used to treat autoimmune diseases.
Surgery: In some infants and children with mutations in the interleukin 10 receptor (IL-10R), bone marrow or stem cell transplantations have proven to be curative therapy.
How we care for IBD
Children and teenagers with IBD have a wide variety of needs that may include various treatments, including medication management, diet modification, growth and development monitoring, surgical care, and psychological support. At Boston Children’s Hospital, we take a team approach to IBD. Because IBD affects more than just the digestive tract, your child’s care team will also include dietitians, social workers, psychologists, and nurse practitioners to help address all aspects of life with IBD.
Inflammatory Bowel Disease | Research & Innovation
Our areas of innovation for IBD
While treating children and teens with IBD is an important part of our mission, we are also committed to researching the biological causes of Crohn's disease and ulcerative colitis. By closely studying these diseases, we are better able to provide our patients with the best understanding of IBD; and with the latest treatment approaches.
Patients who receive care at Boston Children’s have access to the latest clinical trials by a team of specialists at the forefront of discovery. Our investigators are also involved in pioneering research to discover the cause and a cure for VEO-IBD. The center’s director, Dr. Scott Snapper, is a founding member and principal investigator for the U.S. location of the VEO-IBD Consortium, a global network of pediatric gastroenterologists and scientists working to unravel the molecular basis for VEO-IBD and develop better treatments.
Inflammatory Bowel Disease | Frequently Asked Questions
Crohn’s disease and ulcerative colitis are the two main types of inflammatory bowel disease. Within IBD, the split is about half and half.
|
Crohn’s disease |
Ulcerative colitis |
|
Can affect any part of a child’s intestinal tract |
Affects the colon, and very occasionally the lowest part of the small intestine |
|
Symptoms include diarrhea, bleeding, abdominal pain, tiredness, fever, fatigue, anemia, or weight loss |
Symptoms usually include abdominal cramps and diarrhea with bleeding |
|
Can affect the entire thickness of the intestinal wall |
Involves only the innermost lining of the intestinal wall |
|
Can affect different segments of the intestine, “skipping” some in the middle |
Inflammation typically does not “skip” sections of the intestine |
Crohn’s can be more challenging to treat because it can involve many different areas of the intestine. And since the symptoms are more subtle, it sometimes takes more time to diagnose.
Approximately one out of 10 children has indeterminate colitis, which means that the doctor can’t definitively state whether the disease is ulcerative colitis or Crohn’s, even after thorough medical testing. Over time, many cases of indeterminate colitis will ultimately be diagnosed as either ulcerative colitis or Crohn’s. This is treated similarly to Crohn’s and ulcerative colitis.
Even though they have similar symptoms, these two conditions are very different:
- IBS doesn’t involve inflammation of the intestine.
- Unlike IBS, the inflammation present in IBD can cause permanent scarring and damage to the intestine that may require surgery.
- Different medications are used to treat IBD and IBS.
- In general, people with IBS don’t have blood in their stool.
Sometimes it’s not clear whether a child who has IBD is experiencing an IBD flare-up or an episode of IBS, and the doctor will perform a colonoscopy to check for inflammation. If inflammation is present, it’s likely to be a flareup of IBD.
Since there is currently no cure for IBD, it’s likely that Crohn’s disease or ulcerative colitis will always be a part of your child’s life. However, researchers are continuing to identify better treatments for these conditions.
Your child will probably have to take medications for the foreseeable future. He or she will also have more doctors appointments than before this diagnosis, and may have to stay at the hospital at some point. Other than that, there’s no reason to think that IBD will restrict your child’s life in any significant way. Many celebrities, famous athletes, and former presidents have had IBD.
No, there is no evidence that IBD is caused by stress. But living with a chronic illness can be stressful, and stress can make your child feel less well or even contribute to a flareup. That’s why it’s best for your child to stay on her medical regimen even when she’s feeling well, and anticipate and prepare for stressful situations.
Good nutrition is necessary to promote growth and development. Your child may notice an increase in symptoms with certain foods, in which case avoiding those trigger foods may help. Certain diets can help decrease inflammation, which can be useful in conjunction with medication. In general, we recommend focusing on fresh fruits and vegetables and lean meats and avoiding high fat, processed foods. Some children with IBD have difficulty with strictures or significant inflammation and may need to adhere to a low-residue diet or avoid foods that could cause an obstruction through the narrowed part of the intestine, such as popcorn, nuts, seeds, and the skin of fruit. Your gastroenterologist will tell you if dietary modifications are necessary.
Generally speaking, no. As long as your child is feeling well enough to participate, physical activity is encouraged. In addition to the many other benefits of exercise, it can also help maintain bone density, which can be very helpful for children with IBD. Your child’s doctor will give you more specific advice about good activities for your child.
Typically, children can manage their IBD at home and do not require hospitalization. Occasionally, a child’s symptoms may be so severe that he or she needs to spend some time in the hospital, so that doctors can correct malnutrition and stop diarrhea and the loss of blood, fluids, and mineral salts.
A flareup is a usually a recurrence of one or more of the symptoms that originally led your child to be diagnosed with IBD (e.g. diarrhea, rectal bleeding, and cramping). Most people with IBD experience an occasional flareup. If your child seems to be showing symptoms of a flareup, it’s a good idea to check with your child’s primary care doctor or gastroenterologist. When a patient is off of steroids and feeling well, they are in remission.
Communication is key when dealing with your child’s school, and it’s a good idea to let them know of the diagnosis as early as possible. It’s important that your child’s teachers know that he or she may need to be excused to go to the restroom suddenly or frequently and may miss school due to illness. The school nurse can usually write a confidential memo to your child’s teachers.
IBD can be hard to discuss sometimes, because many of its symptoms involve things that we don’t normally talk about. But the most important thing is communication — it’s very important that you be able to talk to your child about her condition. Be open about it, and if you’re embarrassed, don’t hide it. It’s also a good idea to learn as much as you can about IBD, talk to people who are in similar situations and try to educate the people who are closest to you about your child’s condition.

